-
PDF
- Split View
-
Views
-
Cite
Cite
Marwan Abboud, Maxim Geeroms, Hiba El Hajj, Nicolas Abboud, Improving the Female Silhouette and Gluteal Projection: An Anatomy-Based, Safe, and Harmonious Approach Through Liposuction, Suspension Loops, and Moderate Lipofilling, Aesthetic Surgery Journal, Volume 41, Issue 4, April 2021, Pages 474–489, https://doi.org/10.1093/asj/sjaa157
Close - Share Icon Share
Abstract
Liposuction is the main technique to improve body contour, emphasize appealing curves, and highlight one’s muscular definition. The number of procedures in which the harvested fat is utilized for gluteal augmentation has greatly increased.
The authors aim to demonstrate their technique in order to obtain a sculpted harmonious body through a safe procedure, as well as review their 101 consecutive cases between 2014 and 2018.
Anatomical guidelines and preoperative markings were provided to guide the 3-step procedure: zones of maximal and mild liposuction, barbed wire suspension, and moderate fat grafting. Novel concepts are introduced as the anterior body diagonal, posterior body diagonal as well as other specific axes the pubic unit, and a vertical ratio for the buttock, which are the basic foundations for sculpting the female body into a pleasing hourglass shape with a well projected buttock. Recommendations for location of sacral diamond, sacral dimples, and the maximally projected point of the buttock are given. The authors explain their philosophy through 4 principles: knowledge of anatomy, the relationship between specific body areas and surrounding zones, a balanced gluteal augmentation is not achieved through large volume fat grafting alone, and grafting in the subcutaneous layer.
A total of 101 patients were treated following the described technique and examples are shown. The complication rate was low. No serious adverse effects were recorded apart from 1 ruptured suspension loop.
The described anatomy-based approach, including liposuction, suspension loops, and fat grafting, is a novel and safe technique leading to a desirable, long-lasting outcome.

Liposuction is utilized to improve body contour, emphasize the patient’s appealing curves, and highlight muscular definition. Because of its versatility and relatively noninvasive character, the liposuction cannula became one of the plastic surgeon’s most valued tools for full body sculpting. During the patient evaluation, one cannot underestimate the importance of creating a balanced shape. Even if the patient consults for a very specific body region, one should keep in mind that restoring body harmony remains the goal in order to avoid an unnatural appearance.
Due to the average patient’s abundant adipose tissues, full body sculpting is a creative game of harvesting fat surplus and transferring it to volume-lacking areas. A specific zone of interest that plays a major role in the convexities and concavities around which our body is built is the gluteal region. Especially during the last decade, an increase in the surgical procedures involving liposuction followed by fat grafting to the buttock has been observed. According to the The Aesthetic Society database, more than 26,000 gluteal augmentations were performed in the United States in 2018, of which 94% were conducted through fat grafting. The number of buttock augmentations increased by 61% over the last 5 years.1
The worldwide plastic surgery community’s attention has been drawn to the complications of gluteal fat grating, including the feared embolization of the injected fat.2-4 Although anatomical studies have helped in understanding the mechanism of the fat embolization and how to avoid it,5,6 the authors also feel urged to search for solutions and find a safer method to obtain the desired volume and projection of the buttock.
This article offers insight into a structured approach utilizing precise preoperative markings that act as a guide to enhance the circumferential silhouette with additional attention to the gluteal area. The authors demonstrate a technique based on power-assisted liposuction, loops and lipofilling that combines liposuction of the back, flanks, abdomen, and thighs; thread suspension of the anatomical creases; and moderate gluteal fat grafting with the aim of achieving a pleasing hourglass shape and a well-projected buttock.
METHODS
Patients and Study Design
A total of 101 female patients who underwent liposuction with gluteal augmentation between December 2014 and December 2018 were evaluated in a retrospective study. All 101 procedures were performed by the same senior surgeon (M.A.). Contraindications were unbalanced diabetes, unstable weight, active smoking, and body dysmorphic disorder. Patients were given detailed information regarding liposuction, suspension loops and fat grafting, and the risks and benefits of alternative surgical options. All patients provided written informed consent. The medical charts and preoperative and postoperative photographs of all 101 patients were reviewed. The study is in accordance with the Declaration of Helsinki guidelines. Approval from an institutional review board or ethics committee was not obtained because all patients underwent surgical procedures in a private practice.
Design
Preoperative markings are performed the evening before the operation and photos are taken. The operative design is marked in a standing position with the feet approximated and the arms adducted. Contour deformities are marked. During the marking process, surgeons are encouraged to interact with the patient to listen to her concerns and personal wishes. The patient’s body is rarely perfectly symmetric, and one should notice the slight asymmetries and discuss them with the patient.
Posterior
The authors start dorsally by marking the vertical midline between the erector spinae muscles (Figure 1A). Both posterior axillary folds (PAF) are connected crossing the vertical midline. The level of the inferior gluteal crease (IGC) is marked, and a horizontal IGC line is drawn below both buttocks. From the PAF, a vertical and straight lateral body line (LBL) is drawn towards the level of the inferior gluteal sulcus. As a result, a rectangle appears on the patient’s trunk. The dorsal midaxillary point (DMP) is being marked between the PAF and the midline. From this point, the posterior body diagonal (PBD) is drawn towards the pes anserinus or goose foot at the medial knee, which is the joint insertion of the sartorius, gracilis, and semitendinosus tendons.
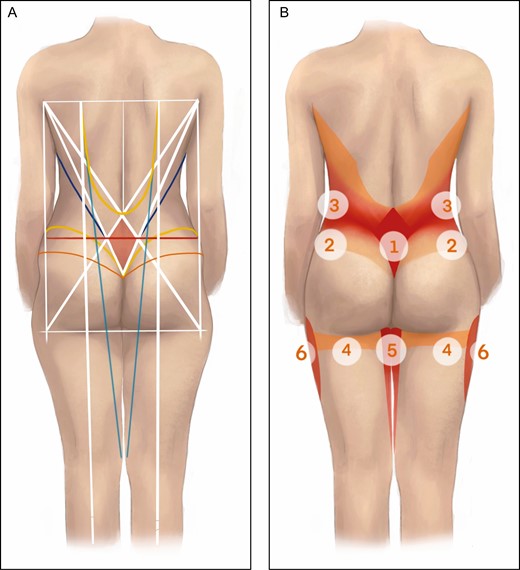
(A) Posterior illustration of trunk, buttocks, and thighs. A rectangle (white) is drawn on the posterior trunk connecting the bilateral posterior axillary fold and bilateral lower lateral buttock. In this rectangle, the sacral diamond (white outline with red center) is determined by drawing the posterior axillary fold-lower lateral buttock and posterior axillary fold-intergluteal crease lines. The ISU line (red) connects the sacral dimples to the sides and towards the umbilicus (red). The desired superior gluteal crease (yellow) is drawn by connecting the intergluteal region to the iliac crest. A line (orange) is drawn from the intergluteal region that extends laterally below the ISU line and above the lateral thigh concavity, indicating tunnelization and lipoaspiration is desired above this level. The posterior body diagonal (turquoise) is drawn by connecting dorsal midaxillary point to the pes anserinus. A vertical dorsal midaxillary point-midpoint of the fossa poplitea axis (white) is designed that determines the horizontal coordinate of the gluteal maximal projection point. An outward-bending trapezius line (yellow) indicates the lateral border of the trapezius muscles and the edge of the liposuction zone. The line connecting the axillary fossa to the ipsilateral sacral dimple (blue) connects the axillary fossa to the ipsilateral dimple. (B) The designed pattern helps to determine zones of liposuction of varying intensity. Maximal aspiration zones are marked in bright red, medium aspiration zones in pink, and minimal aspiration/tunnelization zones in orange. Zones: 1, sacral diamond; 2, posterior lower flank; 3, posterior upper flank; 4, posterior thigh; 5, posterior inner thigh; 6, lateral thigh. ISU, line connecting the indentations at the lateral angles of the sacral diamond with the sides and umbilicus.
Two symmetrical lateral lumbar indentations, which are formed by ligamentous attachments to the posterior superior iliac spines and are referred to as the Venus dimples, are marked. In a typical patient population seeking contour enhancement, the sacral dimples are not always readily visible or palpable. In those scenarios, their position is determined as follows. From the PAF, 2 new lines depart downwards. Firstly, a straight line is drawn towards the upper border of the intergluteal cleft. Secondly, a straight line connects the PAF with the contralateral lower lateral buttock (LLB) at the crossing of the LBL and the IGC line (PAF-LLB line). These bilateral lines create a desirable sacral diamond on the patient’s lower back, which mimics the rhomboid area of Michaelis.7 The diamond’s lateral angles correspond to the sacral dimples, and its inferior angle is positioned at the upper border of the intergluteal cleft. The upper angle is determined by the crossing of the bilateral PAF-LLB lines. This upper angle lies beneath the inferior angle of the trapezius muscle. The resulting diamond overlies the thoraco-lumbar fascia and the tendinous part of the latissimus dorsi muscles. The upper sides run parallel to the tendinous-muscular intersection of the latissimus dorsi muscles. The lower sides overlie the obliquely positioned origin of the gluteus maximus muscle.
The vertical diagonal of the diamond is usually longer than its horizontal diagonal. As a control, this vertical length is divided into 3 equal parts. At the junction of the upper one-third and the lower two-thirds, a horizontal, 10- to 11-cm-long line is drawn (Figure 2). Based on Mahato’s anatomical study of 112 women, Siccardi’s analysis of 30 female pelvises, and pelvimetry by Liselele on 646 women and by Rozenholc on 807 women, the position of the sacral indentation is verified at 5 to 5.5 cm from the midline.8-11
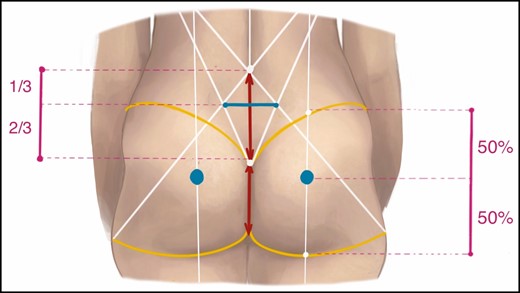
Detail of the sacral diamond (white), which can be located by connecting the posterior axillary fold to the contralateral lower lateral buttock (junction of lower lateral buttock and inferior gluteal crease line) and by connecting the posterior axillary fold to the upper border of the intergluteal crease (white lines). At the junction of the superior one-third and lower two-thirds in this diamond, the dimple location is verified at an approximate horizontal distance (blue line) of 5 to 5.5 cm from the midline (red line). Alternatively, in a patient with visible or palpable sacral indentations, the sacral diamond can be designed by connecting the posterior axillary fold to the ipsilateral dimple as well as by connecting the posterior axillary fold to the contralateral dimple. The ideal point of maximal projection (blue dot) in a buttock is determined at a 50:50 ratio between the upper gluteal edge (level of the iliac crest, yellow) and the lower gluteal edge (yellow) along the vertical dorsal midaxillary point-fossa poplitea line (white).
The indentations (I) at the lateral angles of the sacral diamond are prolonged towards the sides (S) and umbilicus (U), creating the ISU line. Compared with the natural waist, which is situated halfway between the lower rib and iliac crest, the ISU line is located slightly more inferiorly.12The buttock’s footprint is marked as well as a curved line from the upper edge of the intergluteal crease that will join the iliac crest. The authors advise against a merely visual identification of the point of maximal projection on each buttock. A line is drawn from the ipsilateral DMP to the midpoint of the fossa poplitea, which determines the horizontal coordinate. Along this vertical line, the vertical coordinate is determined at an upper buttock to lower buttock ratio of 50:50 (Figure 2). According to Wong’s survey, most women and men from different age groups prefer the buttock’s prominence halfway between the superior gluteal edge (level of the iliac crest) and lower gluteal edge (level of the IGC).13 Ethnic differences and patient preferences should be considered in the determination of the point of maximal prominence.14 Importantly, this marking has to be reevaluated perioperatively because the gluteal height can be shortened enormously during the liposuction.
An outward-bending trapezius line is drawn from the superior edge of the sacral diamond towards the DMP. This line corresponds to the lateral side of the trapezius muscle. From the axillary fossa (AF), the AF-ipsilateral sacral dimple line is drawn towards the ipsilateral dimple at the lateral angle of the sacral diamond.
An inner thigh diamond is drawn over both inner thighs that connects the intergluteal crease superiorly with the PBD laterally and with the pes anserinus inferiorly. This diamond covering the thigh gap has a longer vertical than horizontal axis.
Anterior
The abdominal midline is marked. In analogy to the back, the midpoint between the midline and the anterior axillary fold, the anterior midaxillary point (AMP), is marked (Figure 2A). The AMP is connected to the pes anserinus, resulting in the anterior body diagonal (ABD). The ABD line meets the linea semilunaris and the inguinal fold at the level of the anterior vulvar commissure along its trajectory.
The pubic unit is defined at first (Figure 3B). It starts by drawing a horizontal line at the level of the anterior vulvar commissure that intersects with the inguinal crease. The midpoints between the anterior vulvar commissure and the inguinal crease (point p) are then marked, and a line is drawn between this point and the AMP to define the width of the pubis. The height of the pubis is defined by copying the distance between the 2 points p on the vertical midline line. The pubic unit defined by drawing an AF-PT line from the AF towards the pubic tubercle to mark where lipoaspiration should start to sculpt the pubic unit.
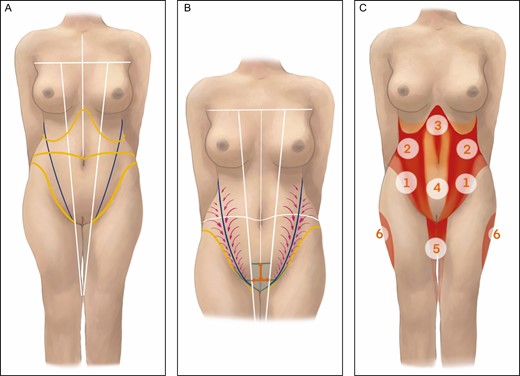
(A) Anterior illustration of trunk and thighs. The vertical midline, anterior axillary fold, and anterior body diagonal connecting the anterior midaxillary point to the pes anserinus are marked (white). The costal border as well as the inguinal crease as part of the PLAISIR line are indicated (yellow). An axillary fold-pubic tubercle line is drawn (blue). (B) A pubic unit (green) is developed by drawing a horizontal line (green) from the anterior vulvar commissure towards both inguinal creases. Halfway between the inguinal crease and the anterior vulvar commissure lies point p. The distance from point p to the midline is measured for both sides (orange). Both distances are added and copied on the midline to determine the superior base of the pubic unit. The connection between the anterior midaxillary point and point p determines the lateral side of the pubic unit. Inside this unit (green) liposuction is discouraged. Lateral to the anterior midaxillary point-p line liposuction is performed to create a pleasing depression, which is in continuation with the PLAISIR line. Further above, maximal liposuction is performed along the axillary fold-pubic tubercle line (purple arrows). (C) The designed pattern helps to determine zones of liposuction of varying intensity. Maximal aspiration zones are marked in bright red, medium aspiration zones in pink, and minimal aspiration/tunnelization zones in orange. Zones: 1, anterior lower flank; 2, anterior upper flank; 3, upper abdomen; 4, lower abdomen; 5, anterior inner thigh; 6, lateral thigh. PLAISIR, line connecting the pubic tubercle, ligamentum inguinale, anterior superior iliac spine, iliac crest, superior gluteal crease, and intergluteal region.
The linea semilunaris is rarely defined in the patient group consulting for body contouring and correlates anatomically with the ABD. The combined left and right rectus abdominis muscles have, instead of a rectangular shape, a slight trapezoid shape with the smallest base inferiorly at the pubic origin and the wider base towards its superior insertion. This narrowing distance between the linea alba and the linea semilunaris from superior to inferior was demonstrated bilaterally by Epstein et al on 18 female cadavers. Briefly, the rectus abdominis muscle has on average a width of 7.1 cm at the umbilical level, 6.0 cm at the anterior superior iliac spine (ASIS) level, and 5.1 cm at the mid-inguinal level corresponding to, respectively, 58%, 49%, and 41% of the horizontal distance between the linea alba and ASIS.15
The costal border is localized, and the ISU line is continued from the posterior side connecting the sacral dimples over the flank to the navel. In patients who underwent abdominoplasty with transposition of the umbilicus, the position of the umbilicus can be too high or too low. It is believed that defining the waist by drawing a circumferential line passing through the posterior dimples is more accurate.
The ligamentum inguinale is marked between the ASIS and the pubic tubercle. A connection is created between the pubic tubercle, ligamentum inguinale, ASIS, iliac crest, superior gluteal crease, and intergluteal region, creating the PLAISIR line.
An anterior inner thigh area is confined over both inner thighs that connects the genital area and medial continuation of the PLAISIR line superiorly with the ABD laterally and to the pes anserinus inferiorly. This zone is in continuity with the posterior inner thigh.
A video showing the preoperative markings is available online as Supplemental Material (Video 1).
Zones
After having drawn the markings, the anatomical liposuction zones can be identified as displayed in Tables 1 and 2.
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| P1. Sacral diamond*** | PAF-LLB lines | PAF-IC lines | Lateral lumbar dimples (if visible/palpable dimples); crossing of PAF-IC line with contralateral PAF-LLB line, 5-5.5 cm from midline at a 1/3 - 2/3 height in sacral diamond (if no visible/palpable dimples present) | — |
| P2. Posterior lower flank** | AF-ID line | Upper buttock and PLAISIR line | LBL | Inferior lateral side of sacral diamond |
| With deep groove | From sacral dimple, along ISU line, toward flank | |||
| P3. Posterior upper flank* | Axilla; PAF-LLB line | AF-ID line | LBL | Superior lateral side of sacral diamond; trapezius line |
| P4. Posterior thigh* | Inferior gluteal crease | 5 cm below the inferior gluteal crease | LBL | PBD |
| P5. Posterior*** | Inferior gluteal crease | Pes anserinus | PBD | — |
| Inner thigh** | ||||
| P6. Lateral thigh** | Lateral and upward continuation of inferior gluteal crease; PAF-LLB line | Junction of middle 1/3 and inferior 1/3 of lateral thigh (adhesion zone) | — | P4 |
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| P1. Sacral diamond*** | PAF-LLB lines | PAF-IC lines | Lateral lumbar dimples (if visible/palpable dimples); crossing of PAF-IC line with contralateral PAF-LLB line, 5-5.5 cm from midline at a 1/3 - 2/3 height in sacral diamond (if no visible/palpable dimples present) | — |
| P2. Posterior lower flank** | AF-ID line | Upper buttock and PLAISIR line | LBL | Inferior lateral side of sacral diamond |
| With deep groove | From sacral dimple, along ISU line, toward flank | |||
| P3. Posterior upper flank* | Axilla; PAF-LLB line | AF-ID line | LBL | Superior lateral side of sacral diamond; trapezius line |
| P4. Posterior thigh* | Inferior gluteal crease | 5 cm below the inferior gluteal crease | LBL | PBD |
| P5. Posterior*** | Inferior gluteal crease | Pes anserinus | PBD | — |
| Inner thigh** | ||||
| P6. Lateral thigh** | Lateral and upward continuation of inferior gluteal crease; PAF-LLB line | Junction of middle 1/3 and inferior 1/3 of lateral thigh (adhesion zone) | — | P4 |
AF, axillary fold; AF-ID, line connecting axillary fossa to ipsilateral sacral dimple; IC, intergluteal crease; ISU, line connecting the indentations at the lateral angles of the sacral diamond with the sides and umbilicus; LBL, lower lateral buttock; LLB, lower lateral buttock; PAF, posterior axillary fold; PBD, posterior body diagonal; PLAISIR, line connecting the pubic tubercle, ligamentum inguinale, anterior superior iliac spine, iliac crest, superior gluteal crease and intergluteal region. *Minimal aspiration/tunnelization zones, **medium aspiration zones, and ***maximal aspiration zones.
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| P1. Sacral diamond*** | PAF-LLB lines | PAF-IC lines | Lateral lumbar dimples (if visible/palpable dimples); crossing of PAF-IC line with contralateral PAF-LLB line, 5-5.5 cm from midline at a 1/3 - 2/3 height in sacral diamond (if no visible/palpable dimples present) | — |
| P2. Posterior lower flank** | AF-ID line | Upper buttock and PLAISIR line | LBL | Inferior lateral side of sacral diamond |
| With deep groove | From sacral dimple, along ISU line, toward flank | |||
| P3. Posterior upper flank* | Axilla; PAF-LLB line | AF-ID line | LBL | Superior lateral side of sacral diamond; trapezius line |
| P4. Posterior thigh* | Inferior gluteal crease | 5 cm below the inferior gluteal crease | LBL | PBD |
| P5. Posterior*** | Inferior gluteal crease | Pes anserinus | PBD | — |
| Inner thigh** | ||||
| P6. Lateral thigh** | Lateral and upward continuation of inferior gluteal crease; PAF-LLB line | Junction of middle 1/3 and inferior 1/3 of lateral thigh (adhesion zone) | — | P4 |
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| P1. Sacral diamond*** | PAF-LLB lines | PAF-IC lines | Lateral lumbar dimples (if visible/palpable dimples); crossing of PAF-IC line with contralateral PAF-LLB line, 5-5.5 cm from midline at a 1/3 - 2/3 height in sacral diamond (if no visible/palpable dimples present) | — |
| P2. Posterior lower flank** | AF-ID line | Upper buttock and PLAISIR line | LBL | Inferior lateral side of sacral diamond |
| With deep groove | From sacral dimple, along ISU line, toward flank | |||
| P3. Posterior upper flank* | Axilla; PAF-LLB line | AF-ID line | LBL | Superior lateral side of sacral diamond; trapezius line |
| P4. Posterior thigh* | Inferior gluteal crease | 5 cm below the inferior gluteal crease | LBL | PBD |
| P5. Posterior*** | Inferior gluteal crease | Pes anserinus | PBD | — |
| Inner thigh** | ||||
| P6. Lateral thigh** | Lateral and upward continuation of inferior gluteal crease; PAF-LLB line | Junction of middle 1/3 and inferior 1/3 of lateral thigh (adhesion zone) | — | P4 |
AF, axillary fold; AF-ID, line connecting axillary fossa to ipsilateral sacral dimple; IC, intergluteal crease; ISU, line connecting the indentations at the lateral angles of the sacral diamond with the sides and umbilicus; LBL, lower lateral buttock; LLB, lower lateral buttock; PAF, posterior axillary fold; PBD, posterior body diagonal; PLAISIR, line connecting the pubic tubercle, ligamentum inguinale, anterior superior iliac spine, iliac crest, superior gluteal crease and intergluteal region. *Minimal aspiration/tunnelization zones, **medium aspiration zones, and ***maximal aspiration zones.
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| A0. Pubic unit**** | p-p distance above anterior vulvar commissure | Inferior edge of labia majora | AMP-p line | — |
| A1. Anterior lower flank** | ISU line | PLAISIR line | LBL | AMP-p line |
| With deep groove*** | Along AF-PT line (oblique) and linea semilunaris (vertical) | |||
| A2. Anterior upper flank** | Costal border; axilla | ISU line | LBL | ABD |
| With deep groove*** | Along AF-PT line (oblique), linea semilunaris (vertical) and costal border (horizontal) | |||
| A3. Upper abdomen* | Costal border; xiphoid process | ISU line | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical), linea alba (vertical), and costal border (oblique) | |||
| A4. Lower abdomen* | ISU line | Pubic unit | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical) | |||
| A5. Anterior*** | Genital area; medial continuation of PLAISIR line | Pes anserinus | ABD | — |
| Inner thigh** |
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| A0. Pubic unit**** | p-p distance above anterior vulvar commissure | Inferior edge of labia majora | AMP-p line | — |
| A1. Anterior lower flank** | ISU line | PLAISIR line | LBL | AMP-p line |
| With deep groove*** | Along AF-PT line (oblique) and linea semilunaris (vertical) | |||
| A2. Anterior upper flank** | Costal border; axilla | ISU line | LBL | ABD |
| With deep groove*** | Along AF-PT line (oblique), linea semilunaris (vertical) and costal border (horizontal) | |||
| A3. Upper abdomen* | Costal border; xiphoid process | ISU line | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical), linea alba (vertical), and costal border (oblique) | |||
| A4. Lower abdomen* | ISU line | Pubic unit | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical) | |||
| A5. Anterior*** | Genital area; medial continuation of PLAISIR line | Pes anserinus | ABD | — |
| Inner thigh** |
ABD, anterior body diagonal; AF, axillary fold; AMP, anterior midaxillary point; ISU, line connecting the indentations at the lateral angles of the sacral diamond with the sides and umbilicus; LBL, lower lateral buttock; PLAISIR, line connecting the pubic tubercle, ligamentum inguinale, anterior superior iliac spine, iliac crest, superior gluteal crease and intergluteal region; PT, pubic tubercle. *Minimal aspiration/tunnelization zones; **medium aspiration zones; ***maximal aspiration zones; ****zones that do not require liposuction.
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| A0. Pubic unit**** | p-p distance above anterior vulvar commissure | Inferior edge of labia majora | AMP-p line | — |
| A1. Anterior lower flank** | ISU line | PLAISIR line | LBL | AMP-p line |
| With deep groove*** | Along AF-PT line (oblique) and linea semilunaris (vertical) | |||
| A2. Anterior upper flank** | Costal border; axilla | ISU line | LBL | ABD |
| With deep groove*** | Along AF-PT line (oblique), linea semilunaris (vertical) and costal border (horizontal) | |||
| A3. Upper abdomen* | Costal border; xiphoid process | ISU line | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical), linea alba (vertical), and costal border (oblique) | |||
| A4. Lower abdomen* | ISU line | Pubic unit | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical) | |||
| A5. Anterior*** | Genital area; medial continuation of PLAISIR line | Pes anserinus | ABD | — |
| Inner thigh** |
| Anatomical zone . | Superior border . | Inferior border . | Lateral border . | Medial border . |
|---|---|---|---|---|
| A0. Pubic unit**** | p-p distance above anterior vulvar commissure | Inferior edge of labia majora | AMP-p line | — |
| A1. Anterior lower flank** | ISU line | PLAISIR line | LBL | AMP-p line |
| With deep groove*** | Along AF-PT line (oblique) and linea semilunaris (vertical) | |||
| A2. Anterior upper flank** | Costal border; axilla | ISU line | LBL | ABD |
| With deep groove*** | Along AF-PT line (oblique), linea semilunaris (vertical) and costal border (horizontal) | |||
| A3. Upper abdomen* | Costal border; xiphoid process | ISU line | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical), linea alba (vertical), and costal border (oblique) | |||
| A4. Lower abdomen* | ISU line | Pubic unit | ABD | — |
| With deep groove*** | Along linea semilunaris (vertical) | |||
| A5. Anterior*** | Genital area; medial continuation of PLAISIR line | Pes anserinus | ABD | — |
| Inner thigh** |
ABD, anterior body diagonal; AF, axillary fold; AMP, anterior midaxillary point; ISU, line connecting the indentations at the lateral angles of the sacral diamond with the sides and umbilicus; LBL, lower lateral buttock; PLAISIR, line connecting the pubic tubercle, ligamentum inguinale, anterior superior iliac spine, iliac crest, superior gluteal crease and intergluteal region; PT, pubic tubercle. *Minimal aspiration/tunnelization zones; **medium aspiration zones; ***maximal aspiration zones; ****zones that do not require liposuction.
Infiltration and Preparation
The subcutaneous tissues are infiltrated with a 0.9% NaCl solution containing 1 mg/L adrenalin for vasoconstriction and 500 mg/L tranexaminic acid (Exacyl).
Bilateral access incisions for infiltration and harvesting were placed as follows: posteriorly: 1 at the upper edge of the intergluteal crease, 1 at the sacral dimple, 1 along the PBD line beneath the bra’s back band, 1 higher up along the PAF-LLB line, 1 along the ISU line, 1 along the superior gluteal border, 1 along the inferior gluteal border at the crossing with the DMP-fossa poplitea line, and 1 in the medial knee region; and anteriorly: 3 in the umbilicus (at 9 hours, 12 hours, and 3 hours), 4 along the ABD line (at the level of the anterior vulvar commissure, at the crossing with ISU line, between the anterior vulvar commissure level and ISU line, and at the crossing with IMF), 1 at the lateral edge of the IMF, and 1 in the medial knee region. Incisions left and right are placed symmetrically to facilitate symmetrical sculpting.
All operations are performed under general anesthesia. Preventive measures are taken to avoid deep venous thrombosis (pneumatic compression garments), pressure sores (adequate padding of pressure points), and hypothermia (warm mattress, heated operation theater, tumescent solution warmed to body temperature, removing spilled tumescent solution from the patient’s body, and convective warming on the nonexposed body parts).
Liposuction in Prone Position
After allowing the tumescent solution to exert its effect for 10 minutes, liposuction is performed utilizing power-assisted liposuction (Lipomatic, Euromi, Liège, Belgium). Fat is always harvested in a fan-like pattern through several access incisions by means of a 3-mm and 4.5-mm multiple-hole cannula attached to a hand piece and set to a negative pressure of 0.7 atm.16
Starting in the prone position (Figure 1B), liposuction is mainly performed to the sacral diamond (P1), posterior lower flanks (P2), posterior upper flanks (P3), and posterior inner thigh triangles (P5). The first step is a thorough aspiration in the sacral diamond (P1) to define the junction between the sacral area and the origins of the gluteus maximus muscles. From a lateral view, it can be monitored how the liposuction starts to visually project the buttock and aims for a desirable lordotic curvature of approximately 45°C between the thoracic back and the buttocks.17 Special attention is given to the diamond’s lateral angles, corresponding to the sacral indentations. A combination of external compression and maximal liposuction with the cannula’s holes facing the dermis removes the fat in this region.
Subsequently, a maximal aspiration is performed along the posterior lower flanks (P2). A gradually increasing aspiration is performed from the upper buttock and iliac crest to the area between PLAISIR line and AF-ipsilateral sacral dimple line to create a concavity along the flank and improve the waist to hip ratio. The maximal aspiration from the sacral diamond is continued laterally starting from the dimples towards the flank. Liposuction should be moderate below the iliac crest and below the PLAISIR line to maintain the hip contour and preserve the shape of the upper buttock. The gluteal and hip preservation combined with the maximal aspiration above the PLAISIR line emphasizes the attractive hourglass shape from a posterior view and the lumbar lordosis from a lateral view.
Lateral from the superior edge of the sacral diamond, the PAF-LLB line, and the curved trapezius line, a more moderate aspiration is advised along the posterior upper flanks (P3). During this part of the procedure, the subcutaneous tissue overlying the trapezius muscle is not harvested. The liposuction should reach up to the axilla.
The posterior thigh (P4) requires tunnelization (passage of the vibrating liposuction device without exerting suction) but is rarely intensively aspirated. Liposuction in the superficial plane of the posterior thigh just below the IGC is optional to highlight the crease and reduce “the banana rolls.” In this particular area, deep liposuction can worsen the buttock’s ptosis, which is difficult to correct.
The upper inner thigh (P5) is aspirated internally from PBD, but below the upper third, liposuction should be more cautious because this area is prone to irregularities.
Below the lower lateral edge of the buttock and along the LBL (P6), a moderate liposuction is performed when volume is lacking in the outer buttock. The goal is not to create a disproportionately narrow thigh base, which would lead to a lollipop deformity, but to achieve a seamless transition, as also pointed out by Vartanian et al.18
After liposuction, the point of maximal gluteal prominence is reevaluated, and often it is noticed how the marked point of maximal projection must be lowered so that it fits the 50:50 ratio again. Starting from the new marking of the maximally projected point, the buttock is then divided into 8 triangular parts with a 45° angle (Figure 4). The upper points reach the curve of the desired superior gluteal crease, which is in continuity with the lower angle of the sacral diamond and with the PLAISIR line. The lower 3 points reach the IGC. Distances towards the point of maximal projection are measured, and symmetry is checked between both buttocks before proceeding to the next step.
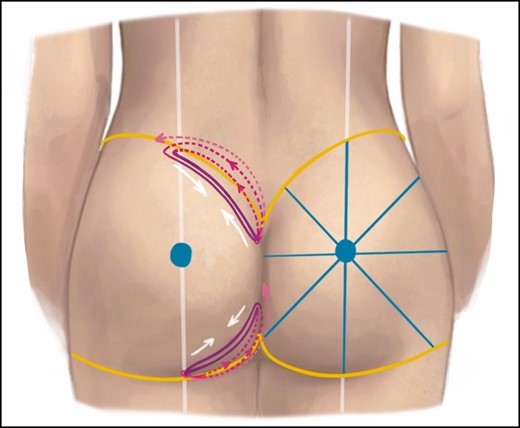
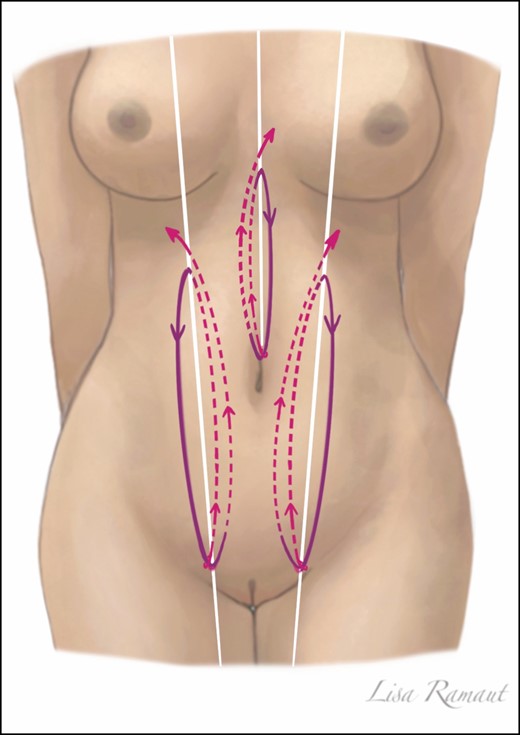
Gluteal suspension loops are placed with resorbable V-loc size 0 barbed wires. Dashed pink lines represent a superficial trajectory of the thread and solid purple lines represent the deeper trajectory. White arrows indicate the effect of the suspension loop. Yellow lines align the superior and inferior gluteal crease after the liposuction. To retrieve the buttock’s point of maximal projection, a vertical axis is drawn from the dorsal midaxillary point towards the center of the fossa poplitea, and a horizontal axis is drawn dividing the vertical axis in half between the superior gluteal crease and inferior gluteal crease. The buttock is divided in 8 parts with angles of 45° which allows to verify the buttock’s symmetry.
Gluteal Suspension Loops
After completion of the liposuction in prone position, the authors utilize glycolic acid and trimethylene carbonate barbed wires with absorption after 180 days (V-loc size 0, Medtronic, Minneapolis, MN) to further increase the definition of the buttocks.
From the lower angle of the sacral diamond, the barbed wire is introduced without the needle in a 3-mm cannula towards the junction of the PBD and the superior gluteal crease. This trajectory is made superficially and corresponds to the medial side of the superior gluteal crease. At the junction, the wire is turned 180° and tunneled in a deeper and slightly lower plane towards the inferior angle of the sacral diamond, where the loop is completed. Subsequently, the wire is tunneled in a slightly higher plane and brought back laterally and superficially along the PLAISIR line. If deemed necessary, the wire can be introduced again (deep) towards the sacral diamond and returned laterally (superficially) for better definition of the crease (Figure 4).
At the level of the IGC, the same type absorbable V-loc 0 is employed. A suspension loop is introduced at the lateral edge of the IGC, which is highly variable among patients. It is then tunneled in a superficial plane towards the most medial part of the IGC, where it exits the skin and is again introduced in a deep plane to the lateral side. The loop is completed as the thread exits the first incision site. Through this first incision site, the barbed loop is suspended medially and upwards in a superficial plane. Again, for a stronger effect, a 4th and 5th passage can be added to create an additional loop. The loop does not extend further laterally from the PBD to prevent widening of the inferior gluteal base width.19,20 The loop is then tightened to shorten the IGC (Figure 4).
Before placing the loops, a tunnelization should be performed of the area above and below the buttocks to dissociate tissue planes, which allows the loops to exert their function in recruiting tissue towards the buttocks and, by consequence, enhance the gluteal volume and visual projection.
Gluteal Fat Grafting
During liposuction, the harvested adipose tissue is collected in a sterile reservoir, transferred to 60-mL sterile syringes, and allowed to decant. The aqueous solution can be easily drained. Prior to the actual fat grafting, the vibrating cannula is passed in a multidirectional and multilayered fashion through the subcutaneous matrix for tunnelization and matrix remodeling to release fibrous bands and increase the recipient area through internal expansion.21
The first area of interest is the deficient midlateral area in the square buttock between the most protruding points of the upper lateral hip and lateral thigh.22 Although this zone can be preoperatively marked for fat injection, gluteal shaping by liposuction of the contour often improves the silhouette substantially and obviates the need for fat grafting. The lower limit of the fat grafting area is defined by the extended straight PAF-LBL line.
Further fat grafting is performed to the zone of maximal projection of the buttock. If the cleavage-like transition from the sacral diamond towards the gluteus maximus muscle origins is not sufficiently defined through liposuction and suspension threads, fat grafting can be performed in this upper medial quadrant, similar to fat grafting to the upper medial breast for fullness. Visible lateral edges of the gluteus maximus muscle can be softened. The fat can be injected in the gluteal subcutaneous tissue by means of the same power-assisted vibration device for maximal dispersion of the fat. This technique combines simultaneous vibration, tunnelization, and grafting. From the syringe, the fat grafting is slowly performed through a 6-mm tube and a custom-made, 3-mm caliber, Y-shaped, 3-hole cannula in a fan-like pattern and in a purely subcutaneous plane avoiding intramuscular grafting.
Whereas the liposuction and fat grafting focus on the subcutaneous fat overlying the gluteus muscles and bony framework, one should also evaluate the patient’s skin quality as the fourth anatomic variable.22 The skin is evaluated for dimpling caused by small herniations of subcutaneous fat. These regions of cellulite are treated by releasing the fibrous septa by performing subcisions followed by fat grafting with small-caliber cannulas. At the end of the liposuction-loops-lipofilling procedure, the eight 45° triangular parts of the buttocks are measured and compared so that asymmetries can be corrected.
A video showing this part of the surgical technique is available online as Supplemental Material (Video 2).
Liposuction in Supine Position
In a second phase of the surgery, the patient is turned to the supine position. The first zone to consider is the pubic unit (Figure 3B). Liposuction is performed beyond the markings of the preoperatively designed pubis to delineate the inguinal groove and create a smooth transition from the pubis towards the umbilicus. The line connecting the AF to the pubic tubercle (AF-PT line) in zones A1 and A2 indicates what should be the deepest groove of the anterior flank (Figure 3B). In analogy with the posterior side, and to maximize the hourglass shape, a gradually increasing liposuction is performed from the PLAISIR line and from the ABD line and axilla towards this groove (Figure 3C).
The tissues overlying the rectus abdominis muscles (zones A3 and A4) are less intensively treated. The A4 and the fat pad in the peri-umbilical region especially are less aggressively aspirated to maintain a natural feminine periumbilical curvature. A maximal liposuction is performed along the relatively avascular linea alba between the xiphoid process and the umbilicus over a width of 2 cm and along the linea semilunaris. Towards the costal borders, more adipose tissue should be aspirated, which can be continued superficially from the lower ribs.
Aspiration of the medial part of the upper leg should focus on the upper fat pad and a progressively tapered thigh line towards the knee. In the middle third of the thigh, superficial liposuction should be avoided to prevent deformities. Aspiration over the adductor area emphasizes the rectus femoris muscle and the sartorius muscle running obliquely from lateral towards a lower medial point. In the lower third of the medial thigh, a convexity is allowed just above the knee corresponding to the medial epicondyle of the femur and the overlying distal part of the vastus medialis and sartorius muscles.
Videos showing this part of the surgical technique are available online as Supplemental Material (Videos 2 and 3).
Abdominal Suspension Loops
To further improve the patient’s abdominal muscular definition, absorbable V-loc 0 is employed. One barbed wire is introduced superficial from the level of the umbilicus to the xiphoid process and brought back in a deep plane to complete a loop to highlight the linea alba (Figure 5). Subsequently, the thread is buried moving upward in a superficial plane.
Abdominal suspension loops are introduced to achieve a better definition of the linea alba and the linea semilunaris. From an inferior incision, the thread is guided in a superficial plane (dashed pink line). The loop is completed by bringing back the thread in a deeper plane (solid purple line) before being transferred back up in a superficial plane.
Similarly, along the lateral border of the rectus abdominis muscle, the barbed wire is inserted superficially above the pubic tubercle and guided upwards toward the costal border. The thread is brought down in a deep plane and the loop is completed before bringing it back up along the ABD. A video showing the utilization of loops in the abdomen and pubis is available online as Supplemental Material (Video 3).
Postoperative Treatment
Access incisions are closed with singular nylon 6/0 sutures. A compressive garment is then applied before the patient recovers from anesthesia and will continue to be worn for 6 weeks. Low–molecular-weight heparin is initiated at a prophylactic dose 8 hours postoperatively and continued depending on the patient’s Caprini risk assessment.23,24 The patient is encouraged to walk as soon as possible. Sitting is allowed in any position without restrictions. Postoperative analgesia consisting of paracetamol (1000 mg, 4×/d) and nonsteroidal antiinflammatory drugs (600 mg of ibuprofen, 3×/d if necessary, with proton pump inhibitor) is administered and continued for on average 1 week. Postoperative massage and lymphatic drainage are important in this area because the lower back tends to retain fluid. Patients received manual lymphatic drainage from day 3 until 2 to 3 weeks postoperatively. Pressotherapy is performed during the same session to further stimulate interstitial fluid reabsorption and lymphatic drainage. Postoperative radiofrequency is prescribed for better skin tightening once per week starting 1 week after the surgery and continued for 5 weeks.
Data Collection and Analysis
Demographic data including age, body mass index, smoking status, and comorbidities such as diabetes, hypertension, dyslipidemia, and other cardiovascular diseases were studied. Postoperative complications were recorded: seroma, infection, necrosis, hematoma, thread extrusion, wound problems, and thromboembolic events. Operative time and fat grafting volume were studied. Postoperative pain was assessed in all patients through the visual analog scale at day 1, day 7, and 1 month postoperatively (mean ± standard error of the mean).
RESULTS
All patients were female aged an average of 36 years (range, 22-53 years). The average operation time was 110 minutes (range, 88-131 minutes from skin incision and excluding the position switch). The average amount of fat injection was 300 mL per buttock (range, 160-620 mL). Not every patient required loops. Some patients refused it and others did not need it after the liposuction. This was based on the operating surgeon’s judgement (M.A.). In total, 83 patients of 101 had suspension loops: 61 of 101 patients required upper gluteal suspension loops, 19 of 101 patients required lower gluteal suspension loops, and 15 of 101 required abdominal suspension loops. All patients left the hospital walking on day 1 postoperative. Average follow-up time was 24 months (range, 10 months to 4 years). The complication rate was low. Except for expected postoperative pain and discomfort, ecchymosis, and burning sensations in the first 2 weeks, no seroma formation, hematoma formation, necrosis, infections, thread extrusions, wound problems, or thromboembolic complications were recorded. Pain was rated 6.4 ± 2.1 on day 1, 3.3 ± 1.0 on day 7, and 0.8 ± 0.4 after 1 month. No suspension loops had to be removed. One patient had a rupture of the upper gluteal suspension loop, leading to an asymmetry, but she did not want to undergo a correction. Clinical cases are shown in Figures 6-7 and Supplemental Figures 1 to 4.
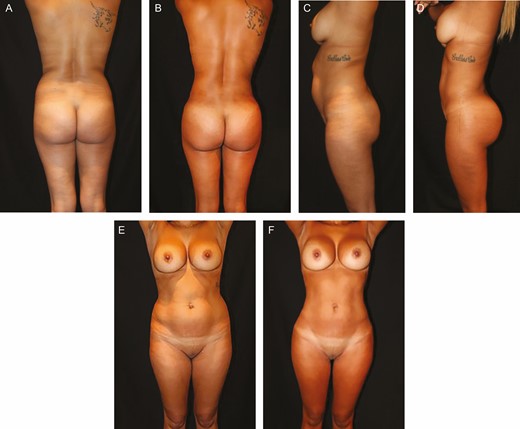
(A, C, E) Preoperative and (B, D, F) 18-month postoperative images of this 34-year-old female patient with a body mass index of 24. The total liposuction volume was 2500 mL, fat grafting volume was 300 mL per buttock, and the gluteal suspension loops were introduced. An improved waist to hip ratio is achieved as well as a shorter gluteal height. Notice how the lateral fulness of the buttock was obtained through fat grafting.
This 36-year-old female patient with a body mass index of 25 previously underwent a 3700-mL liposuction and 600-mL fat grafting per buttock, as previously shown and described in Abboud et al.21 She had a revision surgery 2 years later, during which the authors tunnelized the tissues surrounding the buttocks and introduced the barbed wires for better upper gluteal definition and visual projection. Notice the poorly defined infragluteal folds on the preoperative views and how the addition of suspension loops further improved the gluteal contour. (A, D, G) Before the first surgery, (B, E, H) 2 weeks after the first surgery, and (C, F, I) 1.5 years after the revision surgery.
DISCUSSION
Similar to how a sculptor prepares by drawing before she or he starts carving and modelling, plastic surgeons are guided by their preoperative markings. The authors describe in this article their technique for contouring the anterior and posterior trunk, flanks, buttocks, and inner thighs. Creating the ideal shape of a female body requires a balanced approach, which is obtained through maximal liposuction areas, milder sculpting zones, thread suspension, and fat grafting.
Compared with the authors’ previous work that focused on gluteal augmentation,25 a detailed description was added that acts as a guide to perform a tailored liposculpture in a standardized manner. They introduced the utilization of suspension loops as part of the technique to improve the gluteal and abdominal definition. These barbed wires have multiple advantages. They define natural anatomical landmarks by highlighting a defined junction between the gluteal muscle and the inferolateral part of the sacral diamond. They increase the gluteal projection by recruiting volume towards the buttock, and therefore they decrease the needed volume of fat transfer, which makes the technique safer and more accessible to lean patients with small fat depots who would otherwise require prosthesis placement. The upper gluteal loop emphasizes the appealing lumbar lordosis and acts as an internal support. Apart from recruiting volume towards the buttock and shortening the IGC, the lower gluteal loop has the additional benefit of a lifting effect of the inner thigh. A vibration-assisted tunnelization of the posterior thigh is recommended to allow the lifting process of the posterior thigh skin. The lower gluteal suspension loop aids in curving the lower gluteal fold upwards, leading to a oblique crease that runs superiorly at its medial end of the buttock instead of an unattractive horizontally oriented crease. Furthermore, the loops act as temporary internal binders that maintain tissues in position until healing occurs and better define the limit between the buttock and the back units.
Oh et al26 recently demonstrated a shortening of the infragluteal fold by performing a thread lift with an elastic silicone-polyester thread. The main difference with our technique is the design and goal: whereas we focus on enhancing both the upper and lower gluteal lines and recruiting volume to the buttock’s center, they follow a complete circumferential pattern to moderately lift a ptotic buttock. In our opinion, their circle pattern risks recruiting tissue from the lateral gluteal region, making this area more concave. No tunnelization of the tissues is performed, which negatively influences the long-term results according to our experience. Another difference is their utilization of a permanent thread. Ballivian Rico et al also employ permanent material (ie, strips from a polypropylene surgical mesh) to lift the buttock.27 In our technique, V-loc suspension loops resorb after 6 months, and our definitive results rely on the naturally occurring tissue fibrosis. De Benito et al28 based their 2-stage gluteopexy utilizing sutures with absorbable cones on the same theory that fibrous scar tissue sufficiently develops to support the tissues.
An increasing number of patients consult us for gluteal augmentation. However, with the introduction of the suspension loops and a thorough liposuction including maximal aspiration above the PLAISIR line, the need for large-volume fat grafting is often obviated. This in turn reduces the complication rate2,3 and avoids overloading the graft recipient site of the buttock, which would otherwise lead to potential fat necrosis. By consequence, over the years the technique shifted from extensive gluteal fat grafting combined with moderate liposuction of the surrounding tissues towards a more thorough liposuction of the surrounding area combined with moderate grafting of on average 300 mL fat.
The importance of full body liposuction is highlighted in what is presented as a new ratio (Supplemental Figure 3): the vertical length of the gluteal crease divided by the vertical length of the gluteal height (from superior gluteal crease to IGC). The former will not change much after the surgical procedure; however, the latter can decrease tremendously through intensive liposuction, which will increase this ratio towards a desirable 0.5-0.7 ratio. Together with the ideal waist-to-hip ratio of 0.60-0.65 as advocated by Wong et al,13 these ratios allow to determine, respectively, the ideal vertical and horizontal diameters of the buttocks. It is only through thorough liposuction of the flanks and lower back that the patient’s body can be transformed and these esthetically appealing ratios can be achieved.
Mendieta has described a different buttock height by dividing the sacral height, from L5-S1 to the superior end of the intergluteal crease, by the length of the intergluteal crease.22 Ratios between 0.5 and 1.0 are deemed ideal, especially if one-third to one-quarter of the buttock extends above the intergluteal crease and if one-third to one-quarter extends below the intergluteal crease. Ratios lower than 0.5 indicate an excessively long intergluteal crease, and ratios higher than 1.0 indicate a crease that is too short. A comparison of the intergluteal crease height with the sacral height is definitely useful, although in our opinion it is preferable to compare the intergluteal crease height with the complete buttock height as we describe (Supplemental Figure 3). In the same Mendieta article,22 the author proposed a classification of 4 gluteal frame types to guide the surgical approach. A square buttock is identified by a vertical line connecting the most protruding point in the upper lateral hip with the most protruding point in the lateral thigh. A depression or concavity between these 2 protruding points is not appealing. If excess fat exists between these 2 protruding points, leading to a lateral convexity, it turns into a round buttock. More fat in the upper lateral thigh leads to an A-shaped buttock. Inversely, a V-shaped buttock has more fat in the upper lateral hip. The latter is considered to be unattractive, but for the ideal shape we must consider patient preferences and cultural differences.
The pubic unit design is introduced with superior base and inferior apex as a no-go zone for liposuction. It is recommended to start the liposuction outside of the unit in a moderate fashion towards the umbilicus and in a more aggressive manner laterally from the unit in the inguinal crease. This helps create a groove instead of an obtuse transition from pubis to thigh.
Since 2014, tranexaminic acid (Exacyl) has been added to our infiltration solution as an off-label application. Tranexaminic acid reduces the activity of plasmin directly and indirectly by inhibiting the transformation of plasminogen to plasmin; consequently, less plasmin will degrade fibrin.29 Its intravenous administration has proven to be safe and effective for minimizing blood loss during liposuction.30,31 Compared with intravenous use, topical administration has an equal or superior efficacy based on several trials,32-36 with the added benefit to reduce systemic exposure. The therapeutic effect of tranexamic acid lasts approximately 17 hours in tissues.37 We have an ongoing controlled trial determining the effect of tranexaminic acid on the outcome.
The proposed technique appeared to be safe. Apart from pain, which was tolerable with conventional analgesics, and ecchymosis, no adverse effects were recorded. Of 83 patients who required suspension loops, 1 patient had a thread rupture leading to asymmetry. In the authors’ opinion, the advantages of placing an additional access point outweigh the disadvantage of creating an additional small scar. Multiple access points allow to perform a liposuction in multiple directions at various depths, which avoids contour deformities. Because of the multi-plane liposuction and because of the postoperative compressive garment, the seroma rate in our series was reduced to 0%.
According to the authors’ philosophy, the key for a successful body contouring with buttock enhancement is understanding the following principles:
A thorough knowledge of the body’s unique 3-dimensional (3D) anatomy and shape is fundamental;
We must take into account the relationship of every specific body area, including the gluteal area, with its surrounding zones to achieve a harmonious balance;
We need to appreciate the fact that gluteal enhancement involves more than merely adding volume to the buttock and that liposuction and loops are just as valuable; and
Most importantly, we should not harm, and therefore we should never graft deep to the gluteus muscle fascia.
Two observations should be made. Although we aim for skin retraction, loose skin can occur after liposuction in the lower abdomen, inner thighs, and other areas. This is not always clear during the preoperative consultation, and the patient must be informed about this issue. In patients of older age, after massive weight loss, with stretch marks, or with general poor skin quality, it is advisable to perform liposuction in combination with skin excision. Secondly, we as surgeons cannot follow our markings blindly but rather we must reanalyze our patient intraoperatively. We must understand the buttock is a confluence of structures and we need to create a smooth transition from 1 zone to another to achieve natural curves.
A validated satisfaction questionnaire would have added power, but no standardized survey regarding satisfaction with buttock reshaping was available, which is a limitation to this retrospective study. The outcome is based on clinical and photographic evaluation. No magnetic resonance imaging or 3D imaging was conducted to objectively evaluate the volume or gluteal projection change or to quantify the fat graft resorption.
CONCLUSIONS
An increasing number of patients are consulting with plastic surgeons for full body liposuction and contour enhancement. It is through careful preoperative planning and drawing, based on anatomic principles, that optimal long-lasting results can be achieved. This paper describes the authors’ design and technique for liposuction, suspension loop placement, and fat grafting, which aids in creating a balanced silhouette.
Acknowledgments
The authors would like to thank Dr L. Ramaut for the artwork.
Disclosures
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES





