-
PDF
- Split View
-
Views
-
Cite
Cite
Mark R Magnusson, Commentary on: The Change of Plane of the Supratrochlear and Supraorbital Arteries in the Forehead—An Ultrasound-Based Investigation, Aesthetic Surgery Journal, Volume 41, Issue 11, November 2021, Pages NP1599–NP1602, https://doi.org/10.1093/asj/sjab077
Close - Share Icon Share
When considering dermal filler injections, the brow and low forehead have been considered an area of high reward but also high risk for intravascular injection and therefore a relative “no-fly zone” especially for the inexperienced. The supraorbital (SOA) and supratrochlear artery (STA) as well as the less consistent superficial paracentral and central arteries are implicated in intravascular injection. Details relating to the transition of the SOA and STA from the orbit to subcutaneous fat and the precise location with respect to discrete ligamentous structures and fascial planes have not been well described and are confusing, in part due to the complexity of the fascial planes in this zone. The authors of this study have set out to clarify the 2- and 3-dimensional (3D) relation of the SOA and STA to these anatomic planes as they pass from deep to superficial.1 Key to understanding their findings and visualizing a potential clinical application is a thorough comprehension of the anatomy.
We have long considered facial anatomy in basic terms of 5 layers from skin to deep fascia/periosteum and are particularly improving our understanding of 3D relations in facial anatomy including not just the horizontal planes and vertically orientated retaining ligaments, adhesion zones, and membranous septa, but also the nuances and variations of the fascial planes within different regions.
The forehead follows the general principles of facial anatomy. Retaining ligaments connect layer 5 to the dermis utilizing the reticular cutis and are most densely arranged in regions where there is less movement; the soft tissue spaces of layer 4 predominate where movement is greatest, in this instance over the frontal bone. In these areas of movement the connections between layer 5 and the mobile functional unit of layers 1 to 3 are finer, more distensible, and incomplete. Adhesions and septa (compared to ligaments) only retain the superficial musculoaponeurotic system and considerable movement may still occur at more superficial layers.2 These structures are particularly prevalent in the mobile areas of the face such as the periorbital zone, forehead, midcheek, and jawline.
The soft tissue spaces have certain characteristics, including defined membranous boundaries, an absence of vital structures within or crossing the spaces, and retaining structures with vital neurovascular structures changing plane located within the boundaries of the space but not within the space. Within the spaces there is loose areolar tissue with fine fibrous bands that are easily broken down with minimal force, making them useful for surgical dissection or an even distribution of nonsurgical fillers.3 The passage of the SOA and STA from the deep immobile plane of layer 5 at its egress from the orbit to the intimately bound functional unit of the mobile tissues in layers 1 to 3 takes place in proximity to retaining structures for protection from sheer forces. Sullivan has previously described retaining structures around the medial supraorbital region in close proximity to the SOA.4
The fascial planes associated with layer 3 in this area are complex. The galea splits into superficial and deep layers that engulf the frontalis, forming its relatively weak anterior and denser posterior fascia. The deep layer has been called the deep galea by Knize.5 The deep layer, however, is classically described as dividing into multiple layers low in the forehead: one lines the deep surface of the frontalis and orbicularis oculi, another is fused to the periosteum (called the subfrontalis fascia by Cotofana et al6), and between these layers the deep galea divides to envelop and penetrate the galea fat pad and fat pad glide plane separating muscle from the supraperiosteal plane and the deepest layer of the deep galea.5 I will use the term subfrontalis fascia to distinguish this deepest layer fused with periostuem from the immediate submuscular layer of deep galea, which I shall refer to as the deep frontalis fascia. Cotofana et al also demonstrated a thin fatty layer between the frontalis muscle and deep frontalis fascia, and I will refer to this as subfrontalis fat. Low in the forehead, deep to the brow and lateral to the SOA, the submuscular fat is contributed to by the retro-orbicularis oculi fat pad (ROOF). Medial to the SOA the corrugator supercilii occupies much of this space. These fat pads are quite fibrous and distinct in character from periorbital fat which is almost purely adipose tissue. The subfrontalis fascia connects at the orbital rim with the orbital septum and orbicularis retaining ligament6 (Figure 1).

This representation of the sagittal plane through the entry of the supraorbital artery into the forehead helps outline the relationship among the periosteum, fascial planes, fat compartments, superficial muscles, and the supraorbital artery. The supraorbital artery exits the orbit via a notch in this instance, is protected by fascial structures as it passes directly into an immediate submuscular position separated by subfrontalis fat and the deep frontalis fascia from underlying deeper fat, retaining structures and periosteum. The vessel passes vertically at an average 2.3 mm superficial to periosteum throughout the forehead which is very similar to the supratrochlear artery not shown in this plane. ROOF, retro-orbicularis oculi fat; SOA, supraorbital artery.
Knize described the fusion of the deep galea with periosteum 2 to 2.5 cm above the orbital margin as a zone of fixation.5 Moss et al2 looked at the anatomy of fascial attachments in the temple and periorbital area describing the temporal ligamentous adhesion and supraorbital ligamentous adhesion which coincide with the areas described by Knize and were confirmed by Cotofana et al when he described the middle and inferior frontal septa as the superior and inferior boundaries of this zone.6 These connections are between layer 5 (periosteum) and the deep surface of layer 3 (deep frontalis fascia). Knize also describes a glide zone between the deep frontal fascia and subfrontalis fascia within this area with fat penetrated by fibrous components of the fascia between the septa described by Cotofana et al. The lower extent of this fusion is described at about 10 mm above the supraorbital margin. The maximal height indicated by Moss et al was lateral of the orbital midline and inferior to the lateral temporal adhesion; 2 Hwang et al placed this more central in relation to the orbit and related to the position of the ROOF lateral to the emergence of the SOA beneath the lateral two-thirds of the brow.7 The margins of the ROOF are the inferior frontal septum superiorly (as the lower border of the temporal and supraorbital ligamentous adhesions as described by Moss et al2), the orbicularis retaining ligament inferiorly, and the SOA medially6 (Figure 2).
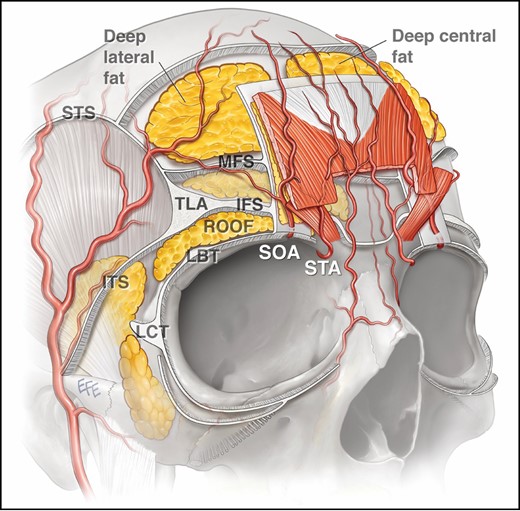
Oblique representation of the fascial and fat compartments of the forehead. By passing directly into the submuscular position deep to orbicularis and frontalis, the supraorbital artery and supratrochlear artery are superficial to the deep fat and corrugator supercilii, inferior and middle septa, deep frontal fascia, and subfrontalis fat. The vessels then change into the superficial position 13-14 mm above the orbital margin. IFS, inferior frontal septum; ITS, inferior temporal septum; LBT, lateral brow thickening; LCT, lateral cantonal thickening; TLA, temporal ligamentous adhesion; MFS, middle frontal septum; ROOF, retro-orbicularis oculi fat; SOA, supraorbital artery; STA, supratrochlear artery; STS, superior temporal septum.
The subfrontalis fascia is fixed by fusion to the periosteum and continues to the orbital margin below, and above to the galea aponeurotica and then occipitalis and finally the occipital bone. The septa described by Cotofana et al connect the periosteum and deep frontalis fascia. The frontalis, however, acts independently of this deep fascial attachment, having no direct bony attachment itself in the periorbital area, and is separated from the deep frontalis fascia by an immediate submuscular fatty layer, comprising subfrontalis fat (Figure 1). In other areas similar fatty planes act as gliding planes for muscle movement. The frontalis goes on to interdigitate with the procerus, corrugator supercilia, and orbicularis oculi as it inserts into the dermis of brow skin. So despite a firm subfrontalis fascial attachment to bone, the superficial layers of the brow are freely mobile under the action of these muscles facilitated by additional fibrofatty planes within layer 3 between muscle (corrugator supercilii, frontalis, and orbicularis oculi) and the deep subfrontalis fascia fused to bone. Consequently, cosmetic injections are still possible deep to muscle without extensive subcision despite deeper fusion between fascia and periosteum, and this is a distinct clinical difference between surgical and nonsurgical anatomy in this area.
The authors of this paper have confirmed that the SOA and STA pass more superficially into layer 2, on average 13 to 14 mm above the supraorbital margin in both sexes with minor variations and this overlies the zone of deep fascial fixation of the subfrontalis fascia to periosteum. Both arteries were coursing deep to the orbicularis oculi (orbital part) muscle immediately after emerging from their respective foramen/notch and then beneath the frontalis as they ascend in the forehead and not within the supraperiosteal plane. The arteries were separated by the deep frontalis fascia from this space and traveled within a thin fatty layer of subfrontalis fat located deep and in immediate proximity to the muscle at a mean distance of 2.3 mm superficial to the periosteum.
When passing a cannula from the lateral brow toward the glabella deep to the orbicularis oculi and frontalis, aiming for the supraperiosteal plane for cosmetic medical procedures, the cannula passes relatively easily just above the supraorbital margin or in the superior elements of the upper lid. A similar easy passage is also achieved in the subgaleal plane of the upper forehead after piercing the lateral temporal adhesion, frontal septa, and superior temporal septum.
The authors conclude that, based on the arterial pathways ascertained in their study, soft tissue fillers can be injected into the supraperiosteal plane of the lower forehead/brow as the arteries are separated by fat and fascia from the target treatment area (Figure 3). Higher in the forehead the subgaleal plane is a safe treatment zone because the SOA and STA pass from deep to superficial at an average of 13 to 14 mm above the superior orbital rim. The superficial plane of the central low forehead should be avoided due to the unpredictable and inconsistent presence of the central and paracentral arteries, which travel in much closer proximity to skin and were identified but were not the immediate target of this study.1
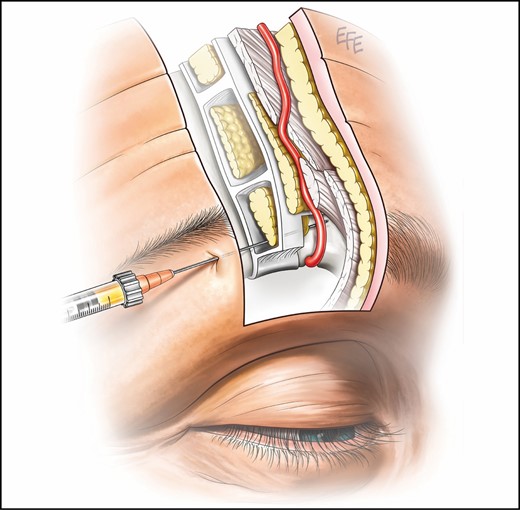
Proposed supraperiosteal plane for filler injection into the brow and low forehead is deep to the retro-orbicularis oculi fat, deep frontalis fascia, and subfrontalis fat separating the vessels from the intended treatment site by 2.3 mm on average.
I congratulate the authors for their ongoing contribution to facial anatomy and specifically helping to further clarify our 3D understanding of this area. I would suggest caution in applying these findings to clinical practice recklessly with a renewed sense of safety without remaining careful and applying all of the principles of safe injecting which I am sure is aligned with the authors’ own feelings. Although the findings indicate a fascial boundary and a layer of fat with more than 2 mm separating the vessels from the periosteum, we are still talking about thin fascial planes in a convex area of the body where the forward passage of a cannula may tend to guide it superficially. Although the anatomy has been freshly illuminated by this study, this same target location has been sought without this knowledge and yet this remains one of the more dangerous zones for cosmetic filler injections and has been responsible for multiple cases of blindness. The anatomy they have uncovered may also explain why blindness is not in fact more common following treatment of this area. An understanding of anatomy is not the only principle for safe injection practices and all principles should be applied, and never more importantly than in these high-risk zones.8
Acknowledgments
Dr Magnusson would like to thank Dr Levent Efe for creating the artwork for this commentary.
Disclosures
Dr Magnusson is an advisory board member for the Allergan Corporation (Dublin, Ireland), is a member of an expert advisory group on breast implants for the Australian TGA, is an editorial board member for the Aesthetic Surgery Journal, was a paid speaker for the Mentor Corporation (2017) and was a founding investor in Strathspey Crown (Newport Beach, CA).
Funding
The author received no financial support for the research, authorship, and publication of this article.
REFERENCES
Author notes
Dr Magnusson is an International Editor for Aesthetic Surgery Journal



