-
PDF
- Split View
-
Views
-
Cite
Cite
Marcos Sforza, Scott Spear, Hybrid Implant and Grafted Fat Breast Augmentation: Designing the Pathway to a Future With Breasts Free of Silicone Breast Implants, Aesthetic Surgery Journal, Volume 41, Issue 11, November 2021, Pages NP1473–NP1485, https://doi.org/10.1093/asj/sjab195
Close - Share Icon Share
Abstract
Fat grafting in breast augmentation surgery is becoming increasingly popular, allowing surgeons to fill the gaps that implant augmentation alone cannot. However, one of the current issues surrounding fat grafting is the lack of standardization.
The objective of this study was to validate and summarize expert-based advice to help plastic surgeons better understand the benefits of utilizing fat grating to reduce implant size in their surgical planning.
This was a prospective study of fat grafting in 56 patients who underwent fat transfer together with silicone breast implants. A 3-dimensional planning system was used to plan the procedure and also to analyze the fat retention and resorption rates. Pictures served as a basis for a questionnaire in which both patients and physicians were asked to rate their satisfaction.
Patients reported a satisfaction rate of “excellent” in 83.3% of cases and “good” in 16.7%. Physician satisfaction was rated as “excellent” in 84.5% of cases, “good” in 13.3%, and “fair” in 4.2% of cases. The mean fat volume grafted per breast was 113.63 mL. The mean absorption rate was 4.53%.
The procedure presented consistent and reproducible results. Hybrid breast augmentation can help design a pathway for a future with breasts free of silicone. This information is particularly relevant for women who have their first breast augmentation at an early age and will probably have 2 to 5 additional surgeries in their lifetime due to the nature of current silicone breast technology.

Plastic surgery is no stranger to controversy, and the subject of infiltrating the breast with fat has been debated repeatedly since its introduction by Neuber over a century ago.1 This dispute is multifaceted—resulting in a range of perceptions regarding popular practice by clinicians.
Autologous fat injection has achieved widespread acceptance over the past 2 decades, being utilized as a soft tissue filler in both small- and large-volume applications.2 This procedure has been widely applied to different regions of the body—most commonly in the face, buttocks, and hands, and to treat postliposuction deformities.
Nevertheless, literature review indicates considerable variability in patient tissue retention following fat injection, leading to numerous unpredictable outcomes, including asymmetry.3,4 With the adverse effects of the procedure being increasingly recognized in the field of plastic surgery, the tendency to use this method in breast surgery, in particular, has decreased.
However, the unifying conclusion of many publications is that there is no Level 1 evidence paper on the subject of fat transfer to warrant a consensus recommendation for clinical practice.5
In this paper, we postulate that a standardized fat transfer procedure will guarantee a consistent and predictable fat retention rate in the group studied. This standardized procedure consists of 4 main principles, as shown in Table 1.
| Procedure . | Description . |
|---|---|
| 1 | Surgical planning preferable with 3-dimensional technology for volume measurement |
| 2 | Harvesting with a small multihole cannula |
| 3 | Processing the fat before injection, with a washing and filtering device |
| 4 | Grafting with a less traumatic technique with small deposits per pass, such as Coleman’s method |
| Procedure . | Description . |
|---|---|
| 1 | Surgical planning preferable with 3-dimensional technology for volume measurement |
| 2 | Harvesting with a small multihole cannula |
| 3 | Processing the fat before injection, with a washing and filtering device |
| 4 | Grafting with a less traumatic technique with small deposits per pass, such as Coleman’s method |
| Procedure . | Description . |
|---|---|
| 1 | Surgical planning preferable with 3-dimensional technology for volume measurement |
| 2 | Harvesting with a small multihole cannula |
| 3 | Processing the fat before injection, with a washing and filtering device |
| 4 | Grafting with a less traumatic technique with small deposits per pass, such as Coleman’s method |
| Procedure . | Description . |
|---|---|
| 1 | Surgical planning preferable with 3-dimensional technology for volume measurement |
| 2 | Harvesting with a small multihole cannula |
| 3 | Processing the fat before injection, with a washing and filtering device |
| 4 | Grafting with a less traumatic technique with small deposits per pass, such as Coleman’s method |
Finally, in contrast to the original composite breast augmentation published by Auclair et al, hybrid breast augmentation is a procedure designed to reduce implant size by utilizing fat grafting in a preoperative, planned fashion to accomplish results equivalent to a larger implant.6 In this paper, we present a prospective study of 56 patients who underwent a hybrid procedure involving fat injections combined with silicone breast implants in a total of 112 breasts. In this study, patients received small- to moderate-volume fat grafts that were harvested, processed, and implanted according to standardized methods. Quantitative 3-dimensional (3D) analysis was applied to obtain reproducible volume retention data.
METHODS
Over a period of 24 months (January 2017-January 2019), 56 female patients presented to our private practice plastic surgery clinic with breasts they perceived as aesthetically unsatisfactory, and sought breast enlargement surgery. Most of these patients had had several consultations at various other plastic surgery clinics before deciding to proceed with surgery. Patients were evaluated and prospectively offered a hybrid procedure with breast implants and autologous fat transfer in an attempt to give them the desired results with smaller implants, as opposed to the larger breast implants originally requested.
The patients ranged in age from 20 to 38 years. The exclusion criteria were patients who smoked, and those with a BMI above 30 kg/m2. None of the patients had existing comorbidities, such as diabetes or high blood pressure. The protocol used in this study was approved by the hospital Medical Advisory Board and this study design was done following the principles of the Declaration of Helsinki. Prior to participation in the study, written informed consent was acquired from all patients.
All patients received subfascial breast augmentation with Motiva SmoothSilk Ergonomix Implants (Establishment Labs, Alajuela, Costa Rica).7,8 After a tumescent infiltration with a standardized Klein solution, fat tissue was then harvested from the abdominal area or thighs—according to patient preference—with a 2.4-mm cannula (Sforza Harvester; Tulip, San Diego, CA) and processed with the Puregraft system (Puregraft LLC, San Diego, CA). After the preparation of the tissue, a double needle-puncture incision was made at 3 and 9 hours on the border of the nipple-areola complex. The calculation of the volume to be inserted was automated and performed by the 3D system according to the authors’ algorithm for hybrid breast augmentation (Figure 1). The surgeon applied the fat in a fan-like movement, with a 10-mL Luer-Lock syringe attached to a 1.2-mm bulb tip cannula (Establishment Labs), aiming to apply 1 mL of fat per passage. Fat grafting was performed until the entire breast was visually covered, as determined by the operating surgeon according to the 3D planning. The volume injected was noted. The total volume of fat transferred per breast ranged from 80 to 158 mL, with a mean [standard deviation] of 113.63 [19.70] mL per procedure. The complete order of the procedure is defined according to the principles shown in Table 1. A narrative video of a similar procedure is available (Videos 1, 2, available online at www.aestheticsurgeryjournal.com).
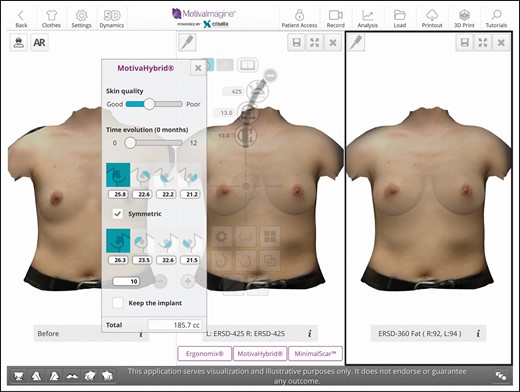
Sample image of a 3-dimensional simulation. (Left) A preoperative image. (Middle) The desired breast size with a 425-cc implant. (Right) A hybrid simulation with a 360-cc implant. The pop-up screen shows the amount of fat to be grafted per breast and per quadrant that was calculated according to the authors’ algorithm. It is interesting to note that the simulation of the hybrid breast and implant-only breast are quite similar, demonstrating to the patient that the equivalent size breast can be achieved with a smaller implant.
All cases were done in a specialized plastic surgery hospital under general anesthesia. All patients signed an informed consent form for the described procedure. All patients received a single dose of 1.5 g of cefuroxime IV as a prophylactic antibiotic 1 hour before the commencement of their operation. Patients wore Preventex compression socks (Covidien, Watford, UK) and a prophylactic pneumatic deep-vein thrombosis system (Flowtron, Malmo, Sweden) during the procedure. However, no chemical prophylaxis for deep-vein thrombosis was given, according to standard hospital policy for short procedures (less than 2 hours). Patients were discharged with compression garments on the harvested area, but wearing only soft bras on the breasts to avoid compression of the transferred fat.
Patients were reviewed at 2 weeks, 6 months, and 1 year post operatively. An ultrasound examination was performed with a 7.5-MHz FDA-registered device at 6 months (Sifsof LLC, Los Angeles, CA). An example scan of a fat-grafted breast is shown in Video 3 (available online at www.aestheticsurgeryjournal.com). Photographs and 3D scans were taken preoperatively, as well as 2 weeks and 1 year postoperatively. The patients were analyzed with a cloud-based 3D imaging software (Crisalix, Lausanne, Switzerland) at all appointments. The 3D analysis provided us with the volume of the breast at 2 weeks and 1 year postoperatively, allowing us to calculate the approximate absorption rates through the postoperative care. It should also be noted that none of the patients in this study received fat grafts in an area with known underlying pathology that might have rendered it more hostile to implanted tissue. For example, none of the patients had received prior radiotherapy or were implanted at an area that had considerable fibrosis and/or physical evidence of impaired vascularity. Four patients did not complete the full follow-up and only 52 were therefore followed for the entire period proposed.
RESULTS
We used the same 1-year patient and physician satisfaction questionnaire validated in our previous publication (Appendixes A and B).9 In total, 52 patients completed the questionnaire. The questionnaires, distributed by a nurse in paper form, were anonymized. At the 1-year time point, patients reported a satisfaction rate of “excellent” in 83.3% of cases and “good” in 16.7%. The 1-year physician satisfaction was rated as “excellent” in 84.5% of cases, “good” in 13.3%, and “fair” in 4.2% of cases. During the follow-up period (2 years), no patients had evidence of seromas or hematomas. One patient (1.9%) had a mild infection of the surgical incision, which resolved with 5 days of ciprofloxacilin 500 mg twice daily. All patients had an ultrasound at 6 months to search for oil cyst formation after fat grafting; no oil cyst formation could be identified in any patient. In all cases, a successful correction of the presenting problem was achieved without complications, as confirmed in the physicians’ questionnaire.
All patients were females who ranged in age from 20 to 38 years old (mean age, 27 [3.68] years). Additional information about patient demographics and complications can be found in Table 2. Multiple regression analysis was conducted to examine the relation between breast volume 1 year post operatively and fat grafting volume, implant volume, and absorption rate as potential predictor variables. The multiple regression analyses yielded a significant model with all 3 predictor variables, F(3100) = 65.33, P < 0.001, accounting for 66% of variance in the final outcome variable. In other words, the 3 independent variables significantly predicted the volume of breast after 1 year, and as expected, a greater volume of fat grafted, larger implants, and low absorption rates guaranteed a larger and more predictable post operative volume.
| Number of patients . | 52 . |
|---|---|
| Number of breasts grafted | 104 |
| Age range (years) | 20-38 |
| Age, mean [SD] (years) | 27 [3.68] |
| Gender | All female |
| Infections | 1.9% |
| Seroma | 0 (0%) |
| Oil cysts | 0 (0%) |
| Hematoma | 0 (0%) |
| Clinically visible rippling | 0 (0%) |
| Capsular contracture | 0 (0%) |
| Displacement | 0 (0%) |
| Number of patients . | 52 . |
|---|---|
| Number of breasts grafted | 104 |
| Age range (years) | 20-38 |
| Age, mean [SD] (years) | 27 [3.68] |
| Gender | All female |
| Infections | 1.9% |
| Seroma | 0 (0%) |
| Oil cysts | 0 (0%) |
| Hematoma | 0 (0%) |
| Clinically visible rippling | 0 (0%) |
| Capsular contracture | 0 (0%) |
| Displacement | 0 (0%) |
SD, standard deviation.
| Number of patients . | 52 . |
|---|---|
| Number of breasts grafted | 104 |
| Age range (years) | 20-38 |
| Age, mean [SD] (years) | 27 [3.68] |
| Gender | All female |
| Infections | 1.9% |
| Seroma | 0 (0%) |
| Oil cysts | 0 (0%) |
| Hematoma | 0 (0%) |
| Clinically visible rippling | 0 (0%) |
| Capsular contracture | 0 (0%) |
| Displacement | 0 (0%) |
| Number of patients . | 52 . |
|---|---|
| Number of breasts grafted | 104 |
| Age range (years) | 20-38 |
| Age, mean [SD] (years) | 27 [3.68] |
| Gender | All female |
| Infections | 1.9% |
| Seroma | 0 (0%) |
| Oil cysts | 0 (0%) |
| Hematoma | 0 (0%) |
| Clinically visible rippling | 0 (0%) |
| Capsular contracture | 0 (0%) |
| Displacement | 0 (0%) |
SD, standard deviation.
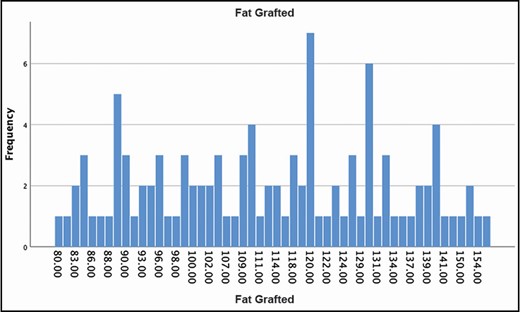
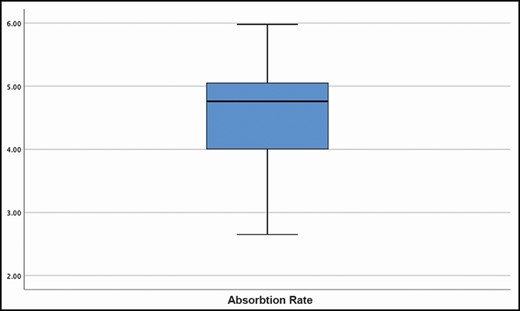
Multiple regression was also applied to examine whether fat graft volume and implant volume are significantly associated with the absorption rate. Statistical analysis of the data revealed that fat grafting volume did not significantly predict the absorption rate, F(1,102) = 0.13, P > 0.05, with this variable accounting for less than 1% of the variability in the data. When implant volume was added as a predictor variable to the model, the analysis still yielded a nonsignificant model for the outcome variable, F(2,101) = 0.18, P > 0.0, accounting for less than 3% of the variability in the data. The findings clearly indicate that the implant and fat graft volumes do not significantly affect the absorption rate. This can be clearly seen in Figures 2, 3. The volume of fat grafted is shown in Figure 4. The mean of volume grafted per breast was 113.63 mL. The mean absorption rate was 4.53%, and a very narrow range of absorption is additionally demonstrated in Figure 5.
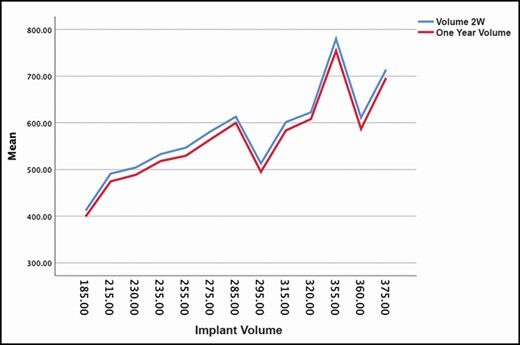
The absorption rate is the distance between the blue and red lines, and remains constant independent of the size of the implant used.
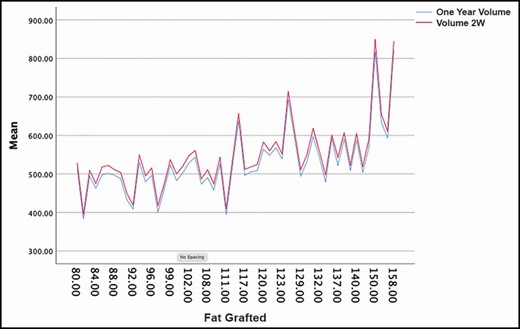
The absorption rate is the distance between the blue and red lines, and remains constant independent of the size of the volume of fat grafted.
Discussion
The current study employed a highly sensitive, objective, and quantitative assessment of volume to examine the rate of tissue resorption following autologous fat grafting. The data demonstrate that a standardized system and method that includes a 3D algorithm, tissue harvesting, processing, and implantation mitigates the vast majority of variability and unpredictability commonly ascribed to autologous fat grafting—such that the volume of tissue implanted is the primary determinant of the absolute amount of tissue volume lost.
Volume Analysis
Ideally, we would like to be able to excise the fat and weigh the specimen, as is done in animal studies, to obtain the most accurate ratio of fat retention. However, because this is not possible in human studies, different types of image-based assessments are utilizied instead. As previously demonstrated by the main author, a validated 3D imaging software is capable of providing accurate numbers and supporting the statistical significance of our results.9 The processing of captured images uses a depth sensor with a precision of around 3 mm at a depth of 1 m (Structure Sensor; Occipital, Palo Alto, CA). In this case, the 3-mm margin is simply a Gaussian error meaning plus/minus, and therefore, when calculating volumes of surfaces, this error will be even smaller or compensated. The system accuracy can demonstrated by, for example, performing 50 consecutive scans of a single patient: the differences in volume variations will always be less than 5% (Figure 6). This method has also been validated by other publications.10
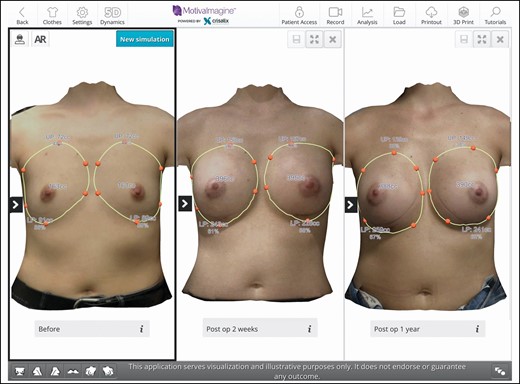
Sample image of a 3-dimensional simulation. (Left) Breast preoperative volume measurement. (Middle) The 2-week total breast postoperative volume. (Right) The 1-year total breast postoperative volume. It is interesting to note that the symmetry of the breasts has improved.
We recognize that such a method has inherent limitations. However, the same applies to any study in which acquired images are used to reconstruct a 3D model. Gerth et al, in their facial fat grafting study, acknowledged that the accuracy of the data obtained with the Vectra 3D system (Canfield, Parsippany, NJ) was user dependent, and errors in volume measurement could be introduced.11
Some studies consider MRI to be an ideal method for volumetric measurements.12-14 However, compared to our portable and affordable 3D technique, MRIs are expensive, time-consuming, and less accessible, especially in private practice.
Fat Absorption vs Total Breast Volume Retention
Another important issue arose during the preliminary evaluations when trying to define the best way to measure volume for this particular work. In our previous work, to assess the predictability of fat grating, we used both preoperative and postoperative volumes to accurately gage the absorption rate.9 As many surgeons have done in the past, we tend to focus on fat retention rates. However, the addition of a breast implant resulted in the need to factor an entirely new range of variables, such as tissue compression, skin stretching, and mass and gravitational impact, into the current study. In reality, when you have a preoperative total breast volume and you add a breast implant, it is very rare for the postoperative volume to be represented by the sum of both measures. Therefore, in order to avoid any information bias, we decided to establish the 2-week total breast postoperative volume as the baseline. The rationale for this baseline was that, after 2 weeks, the effects of the implant addition would be present, and the swelling curve would have passed its peak and would have started descending. This is the most accurate way to evaluate the total breast volume retention rate from 1-year postoperative measurements. We postulated that our method’s findings could be affected by some of the swelling decrease being misinterpreted as fat reabsorption. The alternative would be to use a 6-week data point, when the swelling would be mostly gone, as a baseline. However, it could be argued that the fat would also have started to be absorbed after 6 weeks, resulting in a much lower overall absorption rate. Thus, to avoid the potential of generating positively biased data, we opted to risk the possible aforementioned effect of utilizing the volume 2 weeks postoperation as the total breast volume in our data. Nonetheless, this serves as a support to our widely established and validated method. Perhaps this will lead to a change in the way we measure fat intake because what probably really matters is to what extent the breast can maintain volume over time. Further studies are encouraged to validate such protocols.
Harvest Methodology
The main author has patented the multihole cannula used in this study, and the technology played an important role in explaining the results. The patented cannula has 20 barbed and beveled 1-mm holes arranged in a special layout to facilitate bidirectional harvest. The holes are designed with an elevated 1-mm microport in one end, with the ports at the other end machined with 60° cutting edges. The main author has proved the efficacy of this cannula in a previous peer-reviewed publication.9
In addition, the asymmetric disposition of the holes in a helical pattern ensures all holes receive an identical aspiration pressure. The net effect of the number of holes, in combination with the layout, is to aspirate tissue through all the holes simultaneously. Thus, more fat is harvested with fewer passages, ultimately reducing trauma to the fat and adjacent tissue. By design, the harvested grafted particles are always smaller than 1 mL. Recently, many authors, including Serra-Mestre et al, have adopted this cannula as the standard for fat harvesting and have partially attributed their consistent good results to this device.15 Finally, several studies have demonstrated that larger fat particles tend to have higher absorption rates.16,17
Tissue Processing
The goal of postharvest fat processing is to eliminate contaminants, including cellular debris, free oil, and other nonviable components of the lipoaspirate such as hematogenous cells.18 Inclusion of these contaminants in the grafted material is believed to result in increased inflammation, and thus in lower rates of graft retention.19
In addition to this, many authors believe that maximizing the number of adipose-derived mesenchymal stem cells in the grafted material improves graft viability.20 This belief is based on research demonstrating that adipose-derived mesenchymal stem cells are highly proliferative, and can stimulate regeneration of grafted material by attracting host cells to the graft site.21
This study employed a standardized method for preparing the graft prior to injection. We utilized the Puregraft system to remove contaminants, such as free lipid and fibrotic tissue, from the adipocyte septa white and red blood cells. The washing technique used in this study is efficient for processing larger volumes of lipoaspirate in a feasible time frame.22 We acknowledge that the same instruments and devices may not be available worldwide. However, we believe that standardization is the key to achieving reproducible results. Further studies with other methods of standardization are encouraged.
Free Lipids and Oil Cysts
In a recent paper by Zhu et al, autologous fat grafts prepared with this sterile, single-use approach proved far more effective at removing free lipid, white blood cells, and red blood cells than alternative approaches, such as centrifugation.23 Specifically, the authors reported that free lipids comprised only 0.5% ± 0.1% of the volume of the graft when processed with the Puregraft system, compared with 12.6% ± 1.6% of the volume when the same tissue was processed by centrifugation.
White and Red Blood Cells
In our opinion, the presence of red blood cells will not substantially influence fat intake rates. However, a higher level of red blood cells is thought to be reflected in the amount of postoperative bruising. Although merely a cosmetic feature, less bruising in the immediate postoperative period would help patients feel more confident about their recovery.
Furthermore, the removal of as many white blood cells as possible will certainly be an important factor in reducing local chronic inflammation. Yoshimura et al investigated the detrimental effects, in general, of chronic inflammation from fat grafts, highlighting the possibility of fat absorption and microcalcifications.24
Fibrotic Tissue
The filtration technology we used effectively removes fibrotic tissue from the lipoaspirate. This fibrotic tissue mainly originates from the septa of adipocytes broken during aspiration, to which is eventually added deep dermal tissue when the cannula becomes superficial to the skin. The fibrous tissue takes longer to be integrated and/or absorbed, thus generating a prolonged inflammatory response that can lead to higher fat absorption. Moreover, this tissue can easily suffer calcification that can be misleading in future breast imaging, and therefore it is advantageous to remove as much as possible. Additionally, the importance of oil cysts and calcifications in fat necrosis has been highlighted by various authors, with microcalcifications detected in 25% of cases.25
Tissue Injection (Method and Timing)
All fat was grafted with identical bulb tip small injectors (1.2 mm), without any technical difficulties. Sforza et al have published an extensive study about the performance and safety of these injectors.26 Coleman has reported in detail how multiple injections with small volumes per passage are fundamental to achieving a lower reabsorption rate.12 It should also be remembered that none of the patients received grafts into hostile recipient areas and the grafts were applied subcutaneously. This is noteworthy because it is reasonable to expect a greater percentage resorption at such sites, with these sites being absent in approaches directed at enhancing retention, such as enrichment with stromal vascular fraction cells.27,28
As explained in the description of our surgical technique, fat harvesting is performed after completion of the breast enlargement. We believe that the fat injections should be performed as soon as possible after harvesting and purification in order to improve cell viability.29 Sinno et al have provided a thorough review of the literature in an attempt to differentiate fat grafting fact from fiction; they also consider performing the injections swiftly to be ideal.30 A summary of the principles regarding fat preparation is shown in Table 3.
| “Fresh” fat | Tumescent infiltration at the start of the procedure, succeded by the breast augmentation surgery and then harvesting followed by purification and immediate grafting |
| “Small size” fat | Small aliquots are obtained by harvesting with multihole 2.4-mm or 3-mm cannulas |
| “Good quality” fat | Use a filtration/purification device to try to remove oil, red blood cells, white blood cells, and debris from the lipoaspirate |
| “Standardized” fat injection | Subcutaneous injection in small deposits—Coleman multitunnel injection technique with a bulb tip canula to ensure safety |
| “Fresh” fat | Tumescent infiltration at the start of the procedure, succeded by the breast augmentation surgery and then harvesting followed by purification and immediate grafting |
| “Small size” fat | Small aliquots are obtained by harvesting with multihole 2.4-mm or 3-mm cannulas |
| “Good quality” fat | Use a filtration/purification device to try to remove oil, red blood cells, white blood cells, and debris from the lipoaspirate |
| “Standardized” fat injection | Subcutaneous injection in small deposits—Coleman multitunnel injection technique with a bulb tip canula to ensure safety |
| “Fresh” fat | Tumescent infiltration at the start of the procedure, succeded by the breast augmentation surgery and then harvesting followed by purification and immediate grafting |
| “Small size” fat | Small aliquots are obtained by harvesting with multihole 2.4-mm or 3-mm cannulas |
| “Good quality” fat | Use a filtration/purification device to try to remove oil, red blood cells, white blood cells, and debris from the lipoaspirate |
| “Standardized” fat injection | Subcutaneous injection in small deposits—Coleman multitunnel injection technique with a bulb tip canula to ensure safety |
| “Fresh” fat | Tumescent infiltration at the start of the procedure, succeded by the breast augmentation surgery and then harvesting followed by purification and immediate grafting |
| “Small size” fat | Small aliquots are obtained by harvesting with multihole 2.4-mm or 3-mm cannulas |
| “Good quality” fat | Use a filtration/purification device to try to remove oil, red blood cells, white blood cells, and debris from the lipoaspirate |
| “Standardized” fat injection | Subcutaneous injection in small deposits—Coleman multitunnel injection technique with a bulb tip canula to ensure safety |
The Fear of Breast Cancer
The breast can be augmented or reconstructed in most cases relatively easily with implants or flaps. However, it is important to remember that, in the course of attempts to detect potential disease, the breast is subjected to frequent radiologic and physical examinations, and more than 10% of women eventually develop breast cancer.31 Thus, mimicking, obscuring, or causing breast cancer are concerns that surround any breast procedure or device, and this is particularly true with fat infiltration.
As we assess the value of breast fat infiltration, we need to distinguish 6 different scenarios, assessing them individually and thoroughly more often in the years to come:
Supplementing breast reconstruction by improving contour irregularities
Correcting defects after lumpectomy or other partial injuries
Cosmetic breast enhancement and enlargement, including hybrid approaches aimed at minimizing implant size and better correction of volume asymmetries
Camouflaging implants after breast augmentation
Reconstruction after mastectomy solely by fat infiltration
Hybrid breast reconstruction.
This is why many authors have dedicated their research to clarifying the issues involved.32
Surgeons’ Remarks
A 3D system to plan surgery can provide a great source of accuracy, and the algorithm used in this paper has proven to be able to guarantee high symmetry of breast enlargement based on a precise preoperative volume assessment and an accurate recommendation for the amount to be grafted, considering the variables involved (preoperative volume, implant volume reduction, and predictability of fat absorption rate).
However, if this technology is not available, a simple method for performing hybrid breast surgery can be described as follows:
- •
The breast implant volume (eg, 300 cc) is decided through discussion between the surgeon and patient. The new implant should be 15% to 20% smaller than the original one; 15% would be used for slim patients, and 20% for slightly broader-chested patients. Therefore, the new implant would be between 240 and 255 cc.
- •
The volume of fat to be grafted is then calculated by simply adding 30% to the implant volume removed. This 30% added volume is the average reabsorption rate according to our fat grafting technique.9 In this case, the fat grafted per breast would be around 58 to 78 mL, depending on the implant chosen.
- •
The fat grafted volume can then be distributed equally to the 4 breast quadrants according to the same technique described in this paper.
More than a decade ago, 2 major US meetings (the American Association of Plastic Surgeons and the Northeastern Society of Plastic Surgeons) gave Spear the opportunity to learn at first hand the views plastic surgeons held regarding fat infiltration of the breast.33 Spear reported that the plastic surgeons surveyed overwhelmingly endorsed fat infiltration to complement breast reconstruction, but as a group remained undecided about its use for cosmetic purposes. A clear shift quickly occurred following this, with cosmetic surgery embracing fat grafting worldwide.34
It is clear that if there is a “will,” we are only missing the “way.” The future of hybrid procedures consists in respecting the following basic principles:
- -
Create a concept for hybrid breast augmentation surgery that provides reproducibility, predictability, and better surgical outcomes based on a safe 3D algorithm
- -
Offer a procedure that reduces complications related to volume and silicone weight in breast surgery.
A wide variety of practitioners and industry partners have shed light on the importance of fat graft quality; however, this field is still in its early years in terms of scientific investigations. As we attempt to arrive at our conclusions, we suggest that we should measure and examine 5 factors for every potential application: efficacy, safety, cost, value/work, and liability. While surgeons continue to explore this novel concept and share their experiences on new findings, organized medical societies have the challenging responsibility of preaching caution without stifling progress.
Can hybrid procedures with fat and implants be the new normal? Most importantly, what keeps surgeons sceptical about it? The answer is, as we have described, complex, but it certainly springs from the lack of standardization of such surgeries in the past. With the accelerating speed of scientific advancement and dissemination of knowledge, this responsibility bears more weight and importance. Thus, for highly volatile topics such as this, it may be necessary to review position papers or policy statements more frequently.35
Patients’ Remarks
Results from this investigation can aid in managing patient expectations prior to performing a grafting procedure. Regardless of volume injected, a patient’s perspective of their retained volume will be masked in part by initial swelling and edema. However, the fact that smaller grafts will have a correspondingly small absolute volume of resorption will be difficult to perceive. At the other end of the spectrum, the larger absolute volume of resorption following implantation of a larger graft will be more visually apparent. In this case, there is an increased likelihood that the patient will notice the change, and believe there was poor graft retention. Armed with this knowledge, the surgeon can prospectively inform their patient that perception will vary by volume, thus fostering an enhanced comprehension and avoiding a misunderstanding of expectations. An average hybrid breast augmentation result can be seen in Figure 7 and Supplemental Figure 1 (available online at www.aestheticsurgeryjournal.com).
A 28-year-old female patient shown preoperatively, 2 weeks postoperatively, and 1 year postoperatively. (A-C) Frontal view, (D-F) left side view, and (G-I) right side view.
Drawing the Pathway of a Future Safe Option Without Silicone Implants
Many surgeons would agree that the fate of patients with breast implants will be to have a capsular contracture large-volume breast implant at the end of their lives. Anecdotally, women who have breast augmentations at an early age will almost certainly have further surgeries to replace the devices throughout their lives unless the devices are removed. Moreover, in an attempt to avoid mastopexies when possible, surgeons tend to increase the volume of the replaced breast implants to compensate for any excess skin that has developed with time. This maneuver is reasonable but ultimately does not help the scenario of stretched skin, capsular contracture, and aging .
In our model, the same patient will have her implants reduced in size over time, and the breast tissue will slowly be replaced by her own fat tissue. Eventually, at a mature age, and to reduce the probability of issues with the implants, a simple removal of the now small device combined with a simple fat grafting, if needed, will generally result in a less devastating effect when compared to removing a large breast implant entirely. This is especially true if the patient has had the breast implants throughout her entire adult life—as these would have become a part of who she has grown to be. We vehemently believe that guaranteeing the gradual replacement of silicone by autologous fat tissue is fundamental to ensuring a more aesthetic and natural breast in the years to come. Nonetheless, a breast completely free of silicone after a simple implant removal, but not aesthetically pleasing due to the leftover skin or with scars in an attempt to remove the same excess skin, is the current practice. Our procedure will gradually replace silicone with fat and will almost certainly give patients a much better breast shape after a simple removal. Spear has published extensively on the safety of fat transfer with predictable outcomes and focused the last decade of his career and his personal expertise on studying the safety and enhanced practice methods of the use of fat in breast surgeries.36
This is probably one the first studies to target this specific problem and therefore has an intrinsic limitation related to the number of patients. However, guaranteeing patients the possibility of an old age free of silicone breast implants and with a much more acceptable breast shape is probably one of the fundamental legacies that we can hand over to the generations of patients and surgeons ahead of us.
Conclusions
The results demonstrate, at Level 1 evidence, that this standardized approach provides highly predictable retention outcomes, wherein the percentage of implanted tissue that is lost falls within a very small range and is independent of the absolute volume of tissue implanted. Careful attention to the standardization of tissue collection, processing, and implantation can lead to high predictability of retention of autologous fat grafts in patients with a healthy recipient tissue bed. This predictability can be expected to improve patient satisfaction. This unprecedented endeavor in plastic surgery will sanction a more informed decision-making process, and is a good example of when clinical practice has advanced faster than the supporting evidence accrued so far. In the meantime, it is important to remain open minded and scientifically curious. Most of all, it is important to keep our biases locked up and let the evidence take us where it may.
Acknowledgments
Dr Sforza would like to thank Cindy Spear for reading and acknowledging this work, which both authors started in 2015. She was always the pillar of Scott’s household, family, and practice. Her support was fundamental to allow us to finish a vision, the design of which was started more than a decade ago by one of the most important pioneers of plastic surgery. We will forever miss the great Scott Spear.
Disclosures
Dr Sforza is a member of the Medical Advisory Board of Establishment Labs Inc. (Alajuela, Costa Rica) and an educator for the Motiva Edge platform (Establishment Labs, Alajuela, Costa Rica). Drs Sforza and Spear received compensation for their educational activities for Establishment Labs, Inc.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
References
Author notes
Dr Sforza is responsible for the elective internship in plastic surgery, Dolan Park Hospital, Bromsgrove, UK.
Dr Spear was a clinical professor and was founding professor and chairman of the Department of Plastic Surgery, Georgetown University Hospital, Washington, DC, USA





