-
PDF
- Split View
-
Views
-
Cite
Cite
Sam T. Hamra, Commentary on: Total Composite Flap Facelift and the Deep-Plane Transition Zone: A Critical Consideration in SMAS-Release Midface Lifting, Aesthetic Surgery Journal, Volume 36, Issue 5, May 2016, Pages 546–549, https://doi.org/10.1093/asj/sjw019
Close - Share Icon Share
I must say I was pleased when asked by the editor of this journal to write a commentary when I received the title, 1 since I developed (and named) the composite facelift. Every surgeon who publishes original work wants to see his contribution accepted by his peers. However, I was baffled when reading this article. The technique the author describes is not a composite facelift, as he has entitled his publication. Perhaps the history of the development of the composite facelift 2 will clarify and justify my criticism of this article.
I was fortunate to start with the Skoog rhytidectomy in 1973, 3 and together with Dr. Mark Lemmon we published the only extensive series on Skoog rhytidectomy 4 since Prof. Skoog died in 1974. In 1985, after performing the tri-plane rhytidectomy, which I had published in 1983, 5 I continued to be unhappy with the results. This was essentially an extension of the Skoog rhytidectomy, but with a subcutaneous elevation of cervical skin, since we concluded that the subplatysma cervical Skoog rhytidectomy could not create optimal neck contouring. While the jawline was satisfactory, I felt that the nasolabial fold could be better, and then began working on the technique that I wanted to give an original designation. I called it the deep plane rhytidectomy 6 since it was an extension of the tri-plane rhytidectomy. The concept was relatively simple, as the cheek fat that was between the zygomaticus major and minor was lifted with the skin and kept in continuity with the platysma of the lower face (SMAS). Thus the skin was the vehicle for moving the cheek fat and the SMAS in the traditional lateral direction toward the ear. This original dissection was published, and met with enthusiasm among aesthetic surgeons everywhere.
The result of the deep plane facelift, however, was far short of the harmonious facial rejuvenation that was my goal. I then included the orbicularis oculi muscle in the flap. 7 I named that procedure a “composite rhytidectomy,” since the orbicularis, cheek fat, and platysma never lost their intimate relationship with each other, and the orbicularis was transpositioned in a superior medial vector. The name “composite,” meaning “made of many parts,” was familiar to plastic surgeons who use a composite graft from the ear for nasal reconstruction. Shortly thereafter I published the arcus marginalis release, 8 zygomaticus orbicularis dissection, 9 and the septal reset. 10 These maneuvers created an impressive periorbital rejuvenation, and were the final elements needed to achieve youthful facial harmony. All of these are integral parts of a composite facelift, yet none are referenced by the author. The designation “Composite Rhytidectomy” is an original title, published in 1992 and multiple times thereafter, and should only be assigned to facelifts that accomplish the proven goal.
The textbook I wrote in 1993 on Composite Rhytidectomy 11 was dedicated “to young surgeons who would take this technique and make it better.” Like all plastic surgeons, we try to innovate and create new techniques and publish them, and we are pleased and honored when they are well-accepted and deemed significant contributions. The publication on the deep plane rhytidectomy, the composite rhytidectomy, and the arcus release were listed in an article 12 as three of 50 of the most referenced and significant articles in the past 50 years of aesthetic surgery. It would be difficult to believe that the author was not familiar with the published claims and criteria well known to the world of plastic surgery. His conclusion (“Maintaining skin-SMAS attachments in the DTZ improves midface elevation during SMAS facelifting, exploiting a ‘cantilever bridge’ effect of the skin transferring traction on the SMAS to the malar fat pad.”) is hardly remarkable or novel information.
I can hardly differ with a conclusion that was published as the Deep Plane Facelift in 1990. On the other hand, I object strongly to his use of the title Total Composite Flap Facelift. It is neither total nor a composite facelift flap. It is both misleading and inaccurate. While imitation is said to be the kindest form of flattery, I see this article as deceptive infringement.
The sine qua non of the composite rhytidectomy has been clearly defined. The endpoint must include a high cheek mass, an absent eyelid cheek junction, and a harmonious facial rejuvenation including a forehead lift and neck lift. The author's technique falls far short of these criteria.
The author's description of his surgical technique was essentially published 25 years ago and is a technique many surgeons have modified and published since that time. 13 , 14 It remains essentially a “deep plane rhytidectomy” with results falling far short of a satisfactory comprehensive facial rejuvenation. Even though he states that the orbicularis is included in the flap, the only thing important is the final result, which shows no evidence of orbicularis position change in any of the patients shown in this article. Deep plane facelifts, or malar fat procedures, which are essentially what he has described here, fall under the classification of lateral vector facelifts (Figure 1 A), which comprise of a long list including skin lifts, SMAS lifts, SMASectomy, MAC lifts, FAME lifts, High SMAS lifts, Extended SMAS lifts, and multiple other titles both scientific and marketable. A true composite rhytidectomy (Figure 1 B) is classified as contralateral, quite the opposite of the surgery described in this article.
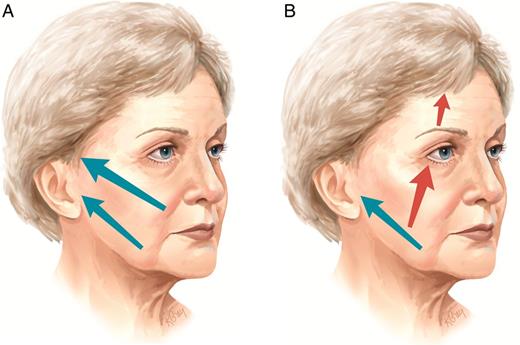
(A) The direction of all lateral vector facelifts. (B) The direction of contralateral composite facelifts.
All lateral vector facelifts share two unfavorable characteristics in common. The first is the lack of true periorbital rejuvenation. This is obvious in all of the author's patient photographs. Note the author's Supplementary Figure 4 (Figure 2 in this Commentary).
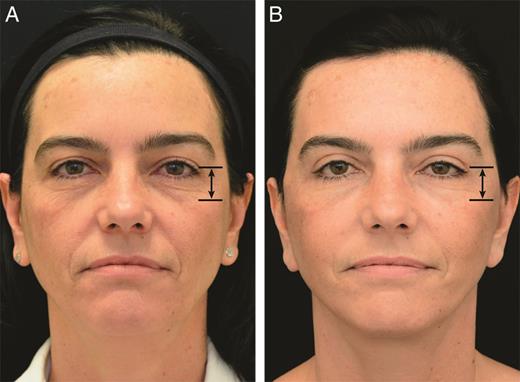
Preoperative (A) and 12 month postoperative (B) photographs of a 45-year-old woman from the author's Supplementary Figure 4. The height of the lower eyelid and the eyelid cheek junction are unchanged. From Mani. 1
Careful analysis of this patient reveals that the lower eyelid height stays exactly the same. The junction between the eyelid and cheek stays exactly the same. Even though the author mentions “vertical” lift of the cheek, it clearly did not happen, as documented in his own patient photographs. He describes a suborbicularis dissection, but since he never makes a subciliary incision, the orbicularis cannot be elevated and transpositioned towards the orbit, which must be accomplished to shorten the height of the lower eyelid. Furthermore, careful observation of the nevi of the face would indicate they are in the same position in the preoperative and postoperative photographs. As I concluded in my article on long-term results of deep plane facelifts, the perceived movement of the cheek without a superior medial lift is really lateral, not vertical, and at best temporary. If in fact there is no shortened lower eyelid height along with an absent eyelid cheek junction then one cannot label this a composite flap facelift. Additionally, when a surgeon does a cheek lift as an obligatory part of the composite procedure, then he is obligated to do a medial vector forehead lift. None of the author's patients have even had a forehead lift. However, my patient's photos (Figure 3 ) demonstrate the final result of a composite facelift: harmonious facial rejuvenation. The high cheek mass and absent eyelid cheek junction in this 66-year-old patient are the obligatory endpoints of a composite facelift.
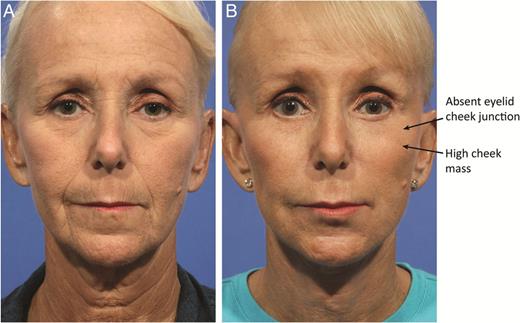
Preoperative (A) and 12 month postoperative (B) photographs of a 66-year-old woman after composite facelift. Note the high cheek mass and the absent eyelid cheek junction.
The second unfavorable characteristic of lateral vector facelifts is the possibility of eventually developing a lateral sweep. Since the SMAS movement and fixation is a short, slightly superior vector, the improved jawline tends to remain repositioned longer than the cheek tissues. As the laterally-secured cheek tissues within a lateral vector flap mature and relax, the cheek fat tends to prolapse inferiorly in the direction of the tightened SMAS tissues, thus evolving into a “facelifted” appearance. This appearance, accompanied by hollow eyes, was described in the 1998 article 15 entitled “Hollow eyes and the lateral sweep.” I have no way of knowing the ultimate appearance of the author's cases reported here, but the combination of excluding a forehead lift and performing a lateral vector procedure is not a recipe for a long-term harmonious appearance, as I noted in my own observation of long-term deep plane facelifts. 16 All of the author's submitted postoperative photographs have some degree of hollowness in addition to an unchanged eyelid cheek junction position. If a surgeon asserts that his facelift technique will endure, then how can he explain or arrest the continuation of aging of other parts of the face? You can't have it both ways. A long-lasting lateral-only repositioning creates disharmony with the rest of the face as time goes on. One must remember that the people seen everywhere with a “facelifted” appearance did not initially have that appearance for perhaps the first year or when their photographs were taken, but they ultimately developed the unsatisfactory facial anatomy over time.
Of additional concern are the photographs themselves. It appears that inconsistencies with the photographic technique used by this author have created a number of problems with the before and after images in this article. It should go without saying that consistent, appropriate lighting and precise patient positioning are extremely critical to documenting our surgical results. Additionally, factors such as ambient room lighting, backgrounds, and any reflective surfaces around the patient, including clothing, need to be controlled and consistent as well. Granted, offices relocate, studios upgrade, and cameras and lighting equipment are replaced, but in this case, the apparent changes in the photographic environment between the majority of the preoperative and postoperative photographs seriously compromise their value. If you examine the photographs carefully, the characteristics of the lighting has changed significantly between the before and after images. There is a much “softer” or more diffuse character to the lighting on the after photographs as well as some evidence of changes in the amount and location of the sources of illumination falling on the faces. This might be due to a change in the type of strobe light being used, for example, using an on-camera strobe with an adjustable built-in diffusion control, or changing to a unit with a different type of reflector within the strobe. In several of the images there is evidence of the presence of additional overhead lighting or a surface reflecting light into the patient's face from above the photographer. These particular changes directly affect the presentation of the topography of the face, especially in that critical area of the eyelid cheek junction. Portrait photographers historically use these “tricks of the trade” to minimize “flaws.” In medical photography, we cannot afford to minimize the appearance of any of these elements of the anatomy − especially when we are documenting and studying the results of a surgical or skin care procedure.
Every surgeon who submits articles describing techniques he feels would benefit others must commit himself to describing a technique that is absolutely reproducible to achieve the result that he is advocating. The surgeon's obligation is always to publish an academically valid paper that will have value and meaning to other surgeons. It must be looked on with respect until those claims are eventually deemed refutable by a more advanced procedure, and even then it should take its place in the bibliography and history of that technique with honor. In all due respect, I feel this paper falls short of that criteria.
Disclosures
The author declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The author received no financial support for the research, authorship, and publication of this article.
REFERENCES



