-
PDF
- Split View
-
Views
-
Cite
Cite
Julia K. Terzis, Elliott H. Rose, Sydney Coleman, Robert L. Walton, Aesthetic Considerations Following Facial Reanimation Procedures, Aesthetic Surgery Journal, Volume 26, Issue 1, January 2006, Pages 57–68, https://doi.org/10.1016/j.asj.2005.12.004
Close - Share Icon Share

Julia K. Terzis, MD
Elliott H. Rose, MD
Sydney Coleman, MD

Robert L. Walton, MD
Dr. Terzis: The first patient is a 24-year-old man with right developmental facial paralysis. He had 3 cross-facial nerve grafts in 1988 and a free-muscle graft in 1990. When he appeared for a follow-up visit in 1991, he was unhappy with his deep nasolabial crease and bulky right cheek. He had slight lagophthalmos in the right eye, but did not complain about that (Figure 1, A). Dr. Rose, how would you address his aesthetic concerns?
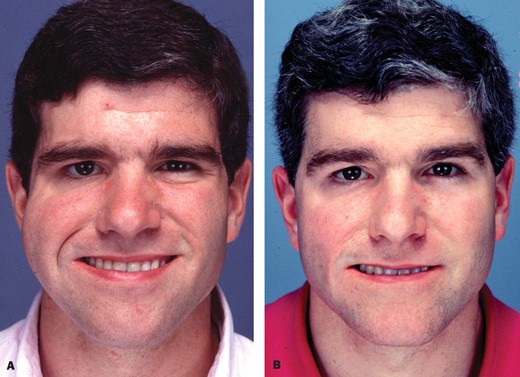
A, This 24-year-old man has right developmental facial paralysis. After undergoing 3 cross facial nerve grafts in 1988 and free gracilis muscle transplantation in 1990, he was unhappy about the deep crease in his right nasolabial fold and a bulky right cheek. B, The patient is shown 7 years after aggressive debulking of the right cheek and placement of a dermal fat graft through an intraoral incision. A mini tendon graft was used to suspend the right lower eyelid.
Dr. Rose: First, he has a beautiful, symmetrical facial reanimation. I have frequently been faced with the problem of a bulky hemi-face, particularly in the zygomatic area of the cheek following free muscle grafts; it presents a particular dilemma. My approach in this patient would be to perform a midfacial advancement through a pre-sideburn incision. I would elevate the right hemi-face and cheek through a face lift plane immediately superficial to the muscle transfer, and very cautiously, under high power magnification, debulk the subcutaneous fat on the surface of the muscle. I would be very hesitant to debulk the muscle itself, since the smile and lateral lip elevation are so symmetrical.
Dr. Terzis: How would you deal with the crease?
Dr. Rose: I would hesitate to disrupt the crease. By performing a midfacial advancement, I would soften the nasolabial fold, thereby minimizing the discrepancy between the fold and the crease. I would not disrupt the fibrous bands at the deep attachment.
Dr. Terzis: Dr. Coleman, this young man is very concerned about the crease. How would you help him?
Dr. Coleman: I would place structural fat grafts into the nasolabial crease in a 2-layered fashion. I have found that in a patient such as this, fat grafts can be placed intradermally with a sharp needle, much like you would use for Restylane (Q-Med, Uppsala, Sweden) or collagen. The intradermal placement would be superficial to the deep placement into the nasolabial fold longitudinally and perpendicularly, using blunt cannulas.
Dr. Terzis: Would you approach it externally or intraorally?
Dr. Coleman: Because I fear contamination, I am reluctant to approach fat grafting intraorally. I almost always approach externally.
Dr. Terzis: What would you do about the bulk? Would you dissect or perform lipoplasty? Also, would you augment the contralateral side?
Dr. Coleman: I think he probably would not like the result if I augmented the contralateral side. I would expect that he does have some superficial fat in the buccal area that would be amenable to debulking with liposuction. In some patients, I might use magnetic resonance imaging (MRI) to find the exact position of the fat before suctioning.
Dr. Terzis: Would you do anything about the increased scleral show of the right eye?
Dr. Coleman: From an aesthetic standpoint, I would consider placing a very tiny amount of grafted fat right under the eyelash to make it more symmetric with the opposite side. This probably will not help with the position of the eyelid but will make the patient happier by providing more symmetry to his lower eyelids.
Dr. Terzis: Dr. Walton, what would you do for the eyelids?
Dr. Walton: In this patient, I would focus on a midface lift with a SMAS suspension. I do not believe the muscle would need to be debulked. However, one may debulk the gracilis muscle fairly liberally without having a problem with the animation. Regarding the position of the commissure and upper lip, I do not believe this can be improved by reinsertion of the muscle. I would perform fat grafting to optimize the contour.
Dr. Terzis: Would anyone consider a dermal fat graft?
Dr. Walton: I have not been uniformly happy with dermal fat grafting in the face. When I have placed a dermal fat graft superficially in the facial soft tissues, I have observed an acneform eruption of the skin overlying the graft. Large grafts tend to calcify and exhibit fat necrosis. Smaller dermis fat grafts, placed deep within the soft tissues, work best. I have been very unhappy with most deeply placed grafts.
Dr. Rose: I have had extraordinary success with dermal strip grafts for vermilion augmentation. I make incisions near the commissure and thread with a tendon passer, placing a strip of dermis submucosally in both the upper and lower vermilion, respectively. I have used this extensively in facial reanimation patients, particularly in those who have had some attenuation of the vermilion from placement of muscles, fascia lata, etc., and it has been a very effective procedure.
Dr. Terzis: Dr. Coleman, do you use dermal fat grafts for contour irregularities following reconstructive procedures?
Dr. Coleman: No, I do not.
Dr. Terzis: Did you try it at one time and, finding it unsatisfactory, then turn to free fat grafting?
Dr. Coleman: Very early in my practice, I used dermal fat grafts several times and found that they were not integrated. They have a tendency to be restrictive, around the mouth in particular.
Dr. Walton: I agree with Dr. Rose's use of dermal fat grafts for lip augmentation. I have had excellent results with this technique. My previous comments related to superficial placement of dermal fat grafts in the facial soft tissues.
Dr. Terzis: This patient was treated by elevation of the right cheek flap through the previous preauricular incision and aggressive debulking of subcutaneous fatty tissue. There was no manipulation of the previously placed free gracilis muscle graft. A dermal fat graft was inserted subdermally at the level of the right nasolabial fold through an intraoral incision. A free mini tendon graft was used to suspend the right lower eyelid. Figure 1, B is a long-term follow-up photo of the patient.
The next patient is a 7-year-old boy with right developmental facial paralysis. In 1989, he had a cross-facial nerve graft, and in 1990, he had a pectoralis minor muscle transfer for the right cheek. His parents brought him back a couple of years later, and he now has a bulky deformity of the right cheek (Figure 2, A). Since this is a pectoralis minor free muscle graft, the cross-facial nerve graft and vascular pedicle are, of necessity, on top of the muscle, not underneath. Dr. Walton, how would you proceed?
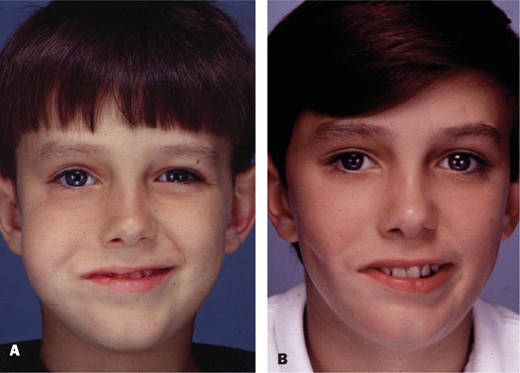
A, This 7-year-old boy has right developmental facial paralysis. He underwent 4 cross facial nerve grafts and a left pectoralis minor muscle transfer to the right cheek. His parents are now concerned with his bulky right cheek. B, The patient is shown several years after aggressive debulking of the right cheek through a preauricular incision.
Dr. Walton: I think the muscle vector might be readjusted to achieve a more vertical pull, the commissure raised, and the nasolabial crease repositioned. I would trim the edge of the muscle judiciously.
But for now, I would leave it as is. This is a young child, and even though he may have excess fat in the cheek, he is still growing, and we do not know how these soft-tissue relationships will change over time.
Dr. Terzis: Are you more inclined to debulk the muscle rather than look for extra fatty tissue to debulk?
Dr. Walton: In this patient, I am not sure that there is excess facial fat. I would need to examine the patient and evaluate his facial animation. My focus would be to reposition the muscle and attempt to create a symmetric nasolabial crease.
Dr. Terzis: Would you do anything to improve his increased scleral show?
Dr. Walton: At this point, I do not think I would. Most of these congenital palsies do not exhibit problems with eye protection. If he did, I would consider it, but I would wait until he was older.
Dr. Terzis: He has asymmetry in terms of contour, with bulkiness in the right cheek, and his parents are concerned. In developmental paralysis, much effort goes toward addressing parental concerns. The children are usually happy with the way they are. Dr. Coleman, how would you handle this child, assuming there was some parental pressure?
Dr. Coleman: I agree with Dr. Walton that I would not approach this too aggressively, especially if the child was not concerned about it. However, I disagree with Dr. Walton in terms of the amount of fat in the cheek, which looks significant to me. If it bothers the child, I would dissect the area after obtaining MRI confirmation of the amount of fat present.
Dr. Terzis: In patients with asymmetric bulk, would you routinely advise getting an MRI? In Virginia, this adds almost $2800.
Dr. Coleman: Even though it is expensive, I feel safer approaching the patient with MRI results.
Dr. Terzis: Would you do anything for his increased scleral show?
Dr. Coleman: The child is young; I would not do anything.
Dr. Terzis: What would you do to debulk the cheek? Would you suction even though there might not be any fat around the muscle? I have seen the pedicle of the gracilis muscle injured in patients who had lipoplasty of the inner thigh area, and the obturator nerve was totally destroyed. Would you perform lipoplasty or work under direct vision?
Dr. Coleman: I would probably consult you and discuss the case first, but I would most likely perform lipoplasty.
Dr. Terzis: Dr. Rose, considering that the parents are concerned about the bulk, how would you treat this child?
Dr. Rose: Looking at the boy's face, I see symmetry of both zygomatic areas and some excessive fullness in the right buccal area. Based on visual appearance, this seems to be predominantly subcutaneous fat (as opposed to muscle bulk) because a pectoralis minor was used for the reconstruction, which is a relatively thin muscle. Only under pressure from the parents would I consider early localized lipoplasty, particularly in the buccal cheek area. I would reserve any specific facial advancement or direct debulking until the boy had passed puberty.
Dr. Terzis: Dr. Rose, the position of the right modiolus is not symmetrical to the left. Would you do anything to set it back?
Dr. Rose: On the deformed side, I have discussed using a facial sling anchored to the modiolus with superior and inferior tails that are threaded into the vermilion border. Looking at the boy, there appears to be about .5- to 1-cm inferior migration of the modiolus compared with the horizontal axis and the contralateral side.
Dr. Terzis: Would you set the fascia lata blindly? How would you tunnel it?
Dr. Rose: I would tunnel it very carefully under direct vision at a deep subcutaneous plane.
Dr. Terzis: Would you tunnel superficial to or underneath the pectoralis minor?
Dr. Rose: I would not go near the pectoralis minor. I would work at a subcutaneous level, making one judicious incision at the lateral commissure and another behind the temple hairline, and then I would thread the fascial graft with a tendon passer beneath the subcutaneous tunnel interconnecting the 2 incisions.
Dr. Terzis: At the lateral commissure, would you put the incision in the natural vermilion?
Dr. Rose: Yes, at the mucocutaneous border at the “V” of the commissure.1
Dr. Terzis: When there is strong animation, is there facial distortion from the fascia lata?
Dr. Rose: That has not been my experience.
Dr. Terzis: Is there external distortion because the muscles that are under the fascia lata are placed so superficially?
Dr. Rose: There is not. My concern in a boy of this age is that because the fascia lata is such a strong structure, with facial growth, if it is faster than the growth rate of the fascia lata, there may be a bit of upward migration of the lateral lip commissure. In most patients, I would go back after puberty, make an incision at the lateral commissure, and divide the insertion of the fascia lata into the modiolus. By this time, the excursion of the muscle has improved and the fascia lata support is no longer necessary to suspend the lateral lip.
Dr. Terzis: Do you have long-term results? What is the longest you have followed fascia lata placement in the face, where there is a lot of animation?
Dr. Rose: In a study that I recently published,2 we had follow-up to 5 and 6 years in both adults and adolescent children. The results showed that we needed to adjust the tension in 20% of the patients, mostly adults, requiring fascia lata tightening. In 2 preadolescent children who received facial reanimation for brain stem tumors, we had to release the fascia lata postpuberty because of excessive overpull after facial growth.
Dr. Walton: I would consider reinsertion of the transfer. The patient may also have a degree of skin and subcutaneous tissue redundancy, which is typical of long-standing paralysis. Instead of removing fat, one might simply perform a hemi-rhytidectomy to eliminate the fullness of the face to achieve improved symmetry. That would be my approach.
Dr. Terzis: This patient was treated with debulking of the right cheek through a preauricular incision and aggressive removal of fatty tissue under magnification. The previously placed free muscle was not disturbed (Figure 2, B).
The third patient is a 3-year-old boy, born with right developmental facial paralysis (Figure 3, A). He had 3 cross-facial nerve grafts and a pectoralis minor muscle transplant to the right cheek. He has a problem of asymmetry coming from a deep concavity of the right cheek. The muscle is sitting at the zygomatic area, and there are slips that extend to the nasal area, the vermilion, and the modiolus. He has a relatively pleasing smile that when activated deepens the concavity. The parents are quite anxious to have the asymmetry corrected. Dr. Coleman, what would you do?

A, This 3-year-old boy was born with right developmental facial paralysis. He had 3 cross facial nerve grafts and a microneurovascular transfer of the left pectoralis minor to the right cheek. His parents would like to correct the loss of soft tissue and asymmetric bulk and concavity in the right cheek. B, The concavity in the right cheek was treated by a free vascularized posterior calf fascia. The patient also had bilateral otoplasty. He is seen here, in adolescence, nearly 13 years later.
Dr. Coleman: First, tell me, when you feel over the zygomatic area, is the skin right on the bone?
Dr. Terzis: The insertion of the pectoralis minor is attached to the zygomatic arch.
Dr. Coleman: By starting directly against the bone and placing layers of fat, the first procedure would cover the entire area of deficiency, which appears to extend from the muscle all the way down to the border of the mandible, and it even looks like the deficiency might extend to the preauricular region.
Dr. Terzis: Can you be more specific in this case about the placement of the fat? Where would you be taking it from, and how much can you insert at the first phase?
Dr. Coleman: In a young man or a young boy, the lateral thigh is the best source. They usually do not have much fat on the abdomen, but occasionally the “love handle” area is a good source. I would start injecting against the bone and layer out into the skin. In this particular patient, I would go from the mid buccal area, almost to the preauricular, to the ear itself, and then down along the border of the mandible.
Dr. Terzis: Would you be placing lines of fat, one after the next, in individual tunnels?
Dr. Coleman: I usually come from 2 directions. In this patient, I would make a small postauricular incision and another incision midway along the border of the mandible and inject lines of fat tissue, radiating out from these 2 directions.
I would be very conservative with the first placement in a patient like this who is still growing. My idea would be to bring him back in a year or so for a second procedure.
Dr. Terzis: How many times do you estimate that you would have to do that?
Dr. Coleman: I might have to treat him from 2 to 4 times.
Dr. Terzis: If you inserted about 5 cc (hypothetically) the first time, how much of this fat do you think would survive?
Dr. Coleman: The real question in someone who is growing and young is what happens to the fat. The answer is that it may survive as fat or survive in some other form.
Dr. Terzis: We know we have 3 months or so in which we lose 50% of the bulk of the free muscle upon transfer. In your experience, do you lose 25% or 50% of the fat? Do you have an approximate figure?
Dr. Coleman: There is much less loss than people think and much greater retention than any of the percentages you indicated. The retention is probably closer to 70% or 80%.
Dr. Terzis: Dr. Rose, what do you think?
Dr. Rose: I would agree with Dr. Coleman that the longevity of fat, particularly in the nonanimated portions of the face, tends to be quite high. My experience is certainly in the 70% or 80% range. In this child, I would strongly consider autogenous fat injection into the depressed areas of the face. I would then reassess when he reaches post adolescence or early adulthood, and if there is a substantial contour deformity, I would consider a customized Porex malar implant (Porex Corp., Newnan, GA) placed through an intraoral incision. In terms of donor sites for fat, particularly in female teenagers, my experience is that the inner thigh is a wonderful source, particularly if the abdomen is flat and there is very little lateral trochanteric fat. In our practice, we harvest excessive fat and, after the preparation, freeze it in sterile syringes for up to 3 years. The patient, returning for reinjection, will not have to undergo another anesthesia for fat harvesting.
Additionally, I would certainly perform a bilateral otoplasty. He has a right nostril collapse, and I would consider a fascial sling for right nostril elevation to resuspend the nostril and open the external nares for improved inspiration.2,3
Dr. Terzis: Dr. Walton, how would you approach this patient?
Dr. Walton: The nasolabial crease on the right is not symmetrical with the opposite side. This may relate to a malinsertion of the transfer. I would examine the patient to see if I might be able to change the angle of the nasolabial crease by adjustments to the muscle insertion. For the cheek concavity, I would consider a microsurgical fat transfer.
Dr. Terzis: Can you describe the type of free transfer you are referring to?
Dr. Walton: We have performed a number of superficial inferior epigastric flap transfers for facial contour abnormalities, and several of these have been in children. I see no reason why this young patient would not be a candidate for such a transfer. It is very easily performed and incurs minimal aesthetic deformity of the abdomen.
Dr. Terzis: Would you consider a vascularized fascia transfer?
Dr. Walton: No. I do not think that the vascularized fascia would provide adequate bulk. I would replace what is missing. Here, it appears to be subcutaneous fat.
Dr. Rose: I would like to interject. With regard to vascularized transfers, a good alternative to free vascularized fascia or fat transfer would be a temporalis fascial flap based on the temporalis vessels, which I have used in a “turnover book” fashion. It is an excellent anatomic location that is contiguous with the buccal area of the cheek.2
Dr. Terzis: If we assume that the superficial temporal vessels have been used, and we have also used the facial vessels for the pectoralis minor, where would you hook your vascularized transfer?
Dr. Rose: In that instance, I would not use a temporalis fascia turnover flap but consider a free flap anastomosed more proximally into the facial vessels.
Dr. Walton: I would like to make one other comment. The temporalis fascial flaps have their pros and cons, but the greatest disadvantage is the potential for hair loss. In ear reconstructions, up to 15% of patients experience thinning or alopecia of the temporal scalp. So I would not use the temporal parietal flap option for this type of deformity.
Dr. Terzis: The concave contour deficit in the right cheek was treated with a free vascularized posterior calf fascia transfer. In addition, this patient had bilateral otoplasty. Figure 3, B shows the patient nearly 13 years later.
The next patient is an 11-year-old girl with partial facial paralysis secondary to resection of a hemangioma, originally treated in November 1974 when she was 3 months old. In May 1986, she had 3 cross-facial nerve grafts and also had a pectoralis minor transferred to her left cheek. She returns with 2 complaints: First, the bulk that you see on the left cheek, and second, the creases (Figure 4, A). The left modiolus was not retracting in a symmetrical fashion with the contralateral side, the left upper lip was not adequately elevating, and the left lower lip was not depressing in a symmetrical fashion. Dr. Walton, how would you help her?
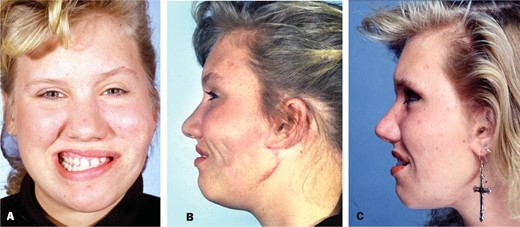
A, B, This young woman suffered left partial facial paralysis secondary to resection of a left parotid hemangioma when she was 3 months old. B, At age 11, she had 3 cross-facial nerve grafts. She then had a free right pectoralis minor transfer to the left cheek. She is currently unhappy with her bulky left cheek and the creases in her left cheek when she animates. C, The patient is seen with the creases effectively corrected by the interposition of a left superficial temporal fascial flap. The left lower lip paralysis was treated by a pedicle left digastric transfer.
Dr. Walton: It appears that there is about 8- to 10 mm of lateral motion of the commissure. There is lack of a vertical animation vector in the upper lip and asymmetry in the smile. Her complaints are bulkiness of the left cheek, secondary to the pectoralis minor. I assume that the neurovascular hilum of the pectoralis minor lies superficial and not deep.
From the frontal view of this patient, I cannot appreciate a major difference in the soft tissue bulk. There is slight asymmetry in the buccal area, but the major appearance problem seems to be in the skin creases overlying the muscle transfer. To resolve the creases, I would interpose a layer of tissue between the skin and the underlying muscle. In this situation, I might use a sheet graft of autologous fat.
Dr. Terzis: Would you inject the creases with the fat tissue?
Dr. Walton: I would place the fat surgically, through a preauricular incision, directly over the muscle. I would change the direction of the muscle or its insertion to optimize the animation of the commissure. I might also consider doing a microneuromuscular unit transfer of the platysma from the opposite side with a neurorrhaphy to the motor branch.
Dr. Terzis: Please clarify; you suggest taking a “free platysma” and bringing it to the other side?
Dr. Walton: I suggest inserting it into the upper lip and the commissure and orienting the motor vector vertically.
Dr. Terzis: Would you vascularize it?
Dr. Walton: Not necessarily. I would place it as a free muscle graft and perform a nerve repair.
Dr. Terzis: Let us turn our attention to the 3 creases on the side of the cheek lateral to the nasolabial fold. These are caused by the interfacing of the free muscle with the overlying skin drape. I have seen such creases in several other patients, especially if they had previous surgery, but I have never seen them in a patient with developmental paralysis. There is also bulk at the level of the pedicle of the pectoralis minor. Dr. Coleman, what would you do about the creases?
Dr. Coleman: I would place fat intradermally by injection with a 22-gauge needle. Then, using a blunt cannula placed in the subcutaneous plane, I would place fat to add more support to each of those creases and separate them from any underlying scar. If that did not relieve them, and if it looked as though there were still an adhesion, I would consider doing subcision. This is a version of the technique that Dr. James Carraway has championed and that dermatologists commonly use to release adherent scars. Basically, one takes a 22-gauge needle and sweeps it through the areas of resistant scarring to break up remaining adhesions.
Dr. Terzis: After you did that, because she might form more scar, more creases, and more adhesions, would you consider injecting some Kenalog (Bristol Myers Squibb, New York, NY)? Or alternatively, would you release the creases and reinforce the area with nonvascularized fat grafts?
Dr. Coleman: I would release the adhesions using the fat grafting. There is a good chance that it would not reattach after free fat grafting. Kenalog injections would be contraindicated.
Dr. Terzis: Would you work with the patient animated or in repose? Would you draw on one side of the face for guidance, or would you have her sustain a smile and then inject?
Dr. Coleman: I could work either way, but I always draw on the face. In an 11-year-old, I do not know if I could use the local anesthesia that would allow her to move or animate.
Dr. Terzis: Dr. Rose, how would you treat her?
Dr. Rose: Adhesions present a particularly difficult problem that I have certainly faced before. They should be approached from both an anatomic and a functional viewpoint. The adhesions are basically dense fiber spans that interconnect the deep dermis to the underlying muscle and restrict excursion. The only way to effectively release them is by direct vision via face lift incision; one can divide the adhesions and completely separate them.
Dr. Terzis: Would you consider an alternative solution such as the possibility of a superficial temporal fascial transfer?
Dr. Rose: Not in this particular patient. It would be overkill—like trying to kill a mosquito with a shovel.
Dr. Terzis: So how would you prevent reformation of the adhesions after you had explored?
Dr. Rose: I reiterate that I would simultaneously harvest autogenous fat, which I then would inject, probably at 6-week and 12-week periods, to correct the dermal imprinting that has occurred from the long-standing adhesions. You could effectively obliterate the dermal indentations by approaching them from a deeper release of the adhesions, as well as superficial filling with autogenous fat. Additionally, the facial skin is redraped at a distant site from the prior adhesions.
Dr. Terzis: Would you do anything about reinserting the modiolus because of the discrepancy between the right and left?
Dr. Rose: When I look at her smile, I cannot just think, as Dr. Walton, that there is a lack of elevation of the superior lip. If you look at the smile, the pull tends to be in an oblique direction, which is reasonably symmetrical to the contralateral modiolus. The deficiency is really in the attenuation of the vermilion on the right upper lip where there is greater show of the teeth. I would put in a dermal strip graft to fill out the vermilion on the right side. The asymmetrical smile is also created by the paralysis of the lower lip depressors. She would be an ideal candidate for the procedure that I have discussed before, which is a platysmal transfer with a fascial extension woven into the orbicularis of the left lower lip.1 This transfer not only statically everts the lower lip, but may also provide some degree of lower lip depression.
Dr. Terzis: The platysma is denervated because of the initial paralysis. Would you still use it as a static suspension?
Dr. Rose: I would not let that deter me from using the platysma for static eversion of the lower lip.
Dr. Terzis: Would you inject the contralateral side with Botox, or would you leave the right lower depressor complex alone?
Dr. Rose: I would first perform the platysma transfer to the left side, assess the “overpull” on the right side, and then consider Botox injections. After a series of Botox injections, if the patient is amenable, then a permanent myotomy could be suggested.
Dr. Terzis: Would any of the other panelists consider using Botox?
Dr. Walton: I would consider Botox. Just a little would level the lower lip, because the lower lip is really pointing down on the right side. If Botox was successful, and she was happy with that, I would consider a permanent ablation of the marginal mandibular branch of the facial nerve.
Dr. Coleman: I might consider using Botox. Again, in an 11-year-old, I would not be too aggressive.
Dr. Walton: I would like to interject. The muscle transfer on the left is not optimally inserted into the modiolus; it is pulling preferentially on the vermilion as opposed to the modiolus and the commissure. That is why you see splaying of the vermilion on the reanimated side. If the transfer was released from the vermilion, an improvement in symmetry would likely result.
Dr. Terzis: I have been very unsuccessful in changing the insertions following free muscle transplantation to the face. I have been very successful in improving symmetry between the normal and the contralateral side by adding additional motor units such as a “mini temporalis.”
The creases in this patient were effectively treated by the interposition of a vascularized left superficial temporal fascial flap between the overlying skin envelope and the underlying free muscle. The left lower lip paralysis was managed by a pedicle left digastric transfer (Figure 4, C).4
The next patient, depicted at age 17, was born in 1969. She had progressive hearing loss, leading to tympanotomy, mastoidectomy, and stapedectomy procedures. Following the stapedectomy in 1977, she suffered complete left hearing loss and complete left facial paralysis. A month later, an ear, nose, and throat surgeon attempted to repair the facial nerve. She presents many years later, in 1986, at age 17 with considerable synkinesis between the left orbicularis oculi muscle and the left commissure when she attempts to smile, but she does not have a complete paralysis; she has a partial paralysis. She had cross-facial nerve grafts and then a right pectoralis minor transfer to the left face. Her deformities include sagging of the left upper lip and a bulky left cheek (Figure 5, A). Dr. Rose, how would you approach these problems?

A, This 17-year-old girl, born in 1969, had progressive hearing loss that led to 2 surgeries in 1976 and 1977 (including left tympanotomy, left mastoidectomy and left stapedectomy) for conductive hearing loss. Following a repeat stapedectomy procedure in 1977, she developed a complete left hearing loss and a complete left facial paralysis. A month later, she had end-to-side coaptation of the left facial nerve. She presented in 1986, at age 17, with left partial facial palsy and synkinesis between the eye and oral sphincters. In 1986, she had 2 cross-facial nerve grafts. In 1987, she had a right pectoralis minor transfer to the left face. She now would like treatment for her bulky left cheek and inadequate elevation of the left upper lip. B, The patient was treated with a left mini temporalis transfer to the left upper lip, and lipoplasty and fat excision in the left cheek to correct the bulk.
Dr. Rose: I would approach the defects in 2 ways. First, I would use a face lift incision to debulk the lower part of the face. Second, with regard to the lack of left upper lip elevation and the inferiorly displaced commissure, I would insert a fascial sling to the lateral lip commissure and modiolus to elevate the modiolus to a neutral horizontal plane. I would also consider improving upper lip elevation. I have not had very good success in trying to redirect the insertion of the muscle. I have, in some of these patients, following a gracilis transfer with lack of elevation in the lip, used a very thin temporalis muscle turnover flap with a fascial extension into the upper lip.
You can take a 1.5- or 2-cm strip, elevate it in an oblique plane that is superior and medial to the original free muscle transfer, and direct it obliquely, not into the lateral lip commissure, but into the lateral third of the upper lip for elevation.
Dr. Terzis: Dr. Rose, you have quite a bit of experience with the use of fascia lata in the reanimation of the face in facial paralysis cases. You said that you usually put the fascia lata strip in the modiolus. Doesn't it get bombarded by the constant contraction of the free muscle?
Dr. Rose: The fascia lata suspension sling is placed in a deeper plane in the face than either the regional muscle transfer or the free muscle transfer. My experience has been that it actually shortens the excursion of the muscle because it does not have to overcome that additional 1 to 1.5 cm of inferior displacement of the lateral lip commissure. So I have found, as an adjunctive procedure to the regional or free muscle transfer, that the autogenous fascia lata sling has been particularly useful.
Dr. Terzis: So if you place the fascia lata strip under tension, and you put it superomedially, doesn't this interfere with the whole cutaneous envelope on top of the free muscle?
Dr. Rose: I think you are misinterpreting the level. I don't put it immediately subdermal in a patient in whom I am concerned about the vascular pedicle. I really place it more at the level of the SMAS.
Dr. Terzis: So you would be putting the fascia lata strip underneath the muscle then?
Dr. Rose: In this patient, I would put it superficial to the muscle because I would not want to run any risk of disrupting either the vascular or the nerve pedicle.
Dr. Terzis: If the pedicle and the nerve are on top of the muscle, where would you place the fascia lata strip?
Dr. Rose: Generally, putting it in either simultaneous with a regional muscle transfer, or at the first stage of a 2-stage free muscle transfer, I have never had the problem of having to avoid the vascular pedicle. I have never had to place it deep to the muscle. In this particular case, you could certainly consider creating a very thin tunnel deep to the muscle, particularly if you knew that the vascular pedicle was on the surface of the muscle.
Dr. Terzis: Dr. Coleman, how would you help this young lady?
Dr. Coleman: The only thing that I would do to help her with her left cheek would be suction.
Dr. Terzis: Would you be able to correct the discrepancy between the right and left upper lip?
Dr. Coleman: The only thing I might consider is adding to the right. Without seeing her mouth in repose it is difficult to be sure, but the mouth probably has significant vermilion excess on the left compared with the right, and with placement of fat into the right lip, the vermilion could be everted to more closely match the left lip.
Dr. Terzis: Dr. Walton, what would you do?
Dr. Walton: The patient has a 3- to 5-mm excursion of the transfer, and the modiolus has been repositioned superiorly 3 to 5 mm. There is still deficiency in the upper lip. I would evaluate and consider repositioning or reinsertion of the muscle transfer to optimize the vector. I think this could be done in lieu of transferring a microneuromuscular unit from the opposite side.
Dr. Terzis: What would you do about the bulk?
Dr. Walton: If the muscle is repositioned, the bulk will not be a big issue. She actually looks like she has subcutaneous atrophy, and the bulk is essentially the muscle in the wrong position.
Dr. Terzis: The bulk, Dr. Walton, is more at the level of the angle of the mandible. I am not aware that I have heard you talk about a reinnervated free platysma or nonvascularized graft. This is an old procedure, but this time with a much more intelligent muscle because it is extremely thin compared with the gracilis. What would you do as far as the modiolus? How would you reposition it in a more acceptable location? The platysma might help the upper lip. Do you think the platysma would also help the commissure?
Dr. Walton: It absolutely would. But the vector has to be correct. You could complement the dynamic animation with placement of a microneuromuscular platysma transfer.
Dr. Terzis: You place the platysma on top of the pectoralis minor and anchor it to the modiolus. Where would you anchor it? Would you go down to the left upper lip? How would you innervate it?
Dr. Walton: I would insert the platysmal transfer in the deep substance of the vermilion cutaneous junction of the upper lip and the modiolus. The muscle would be anchored to the orbital rim.
Dr. Terzis: So, you are talking about a very small strip.
Dr. Walton: Yes, in this particular patient. You have done a nice job of opening the commissure on the affected side, and you have corrected the synkinesis there. I would go with a buccal connection.
Dr. Terzis: Please clarify; what is a buccal connection?
Dr. Walton: This would be a neurorrhaphy between the platysmal nerve branch and a buccal branch of the facial nerve.
Dr. Terzis: This patient was treated with a left mini temporalis transfer placed deep to the previously transferred free pectoralis minor muscle. In addition, she had debulking of her left cheek through a preauricular incision by combination of direct excision of fatty tissue and lipoplasty (Figure 5, B).
References
2
3
4
Author notes
Editor's Note: My thanks to the moderator, Julia K. Terzis, MD (board-certified plastic surgeon and ASAPS member, Norfolk, VA) for developing this discussion as a sequel to the excellent panel “Facial Nerve Injury: Diagnosis and Repair” that appeared in the September/October 2005 issue of Aesthetic Surgery Journal. Thanks also to panelists Sydney Coleman, MD (board-certified plastic surgeon and ASAPS member, New York, NY); Elliott H. Rose, MD (board-certified plastic surgeon and ASAPS member, New York, NY); and Robert L. Walton, MD (board-certified plastic surgeon, Chicago, IL), for sharing their opinions and clinical experience.



