-
PDF
- Split View
-
Views
-
Cite
Cite
Pier Francesco Mancini, A New System for Skin Resurfacing: Preliminary Clinical and Histologic Reports, Aesthetic Surgery Journal, Volume 19, Issue 6, November 1999, Pages 459–464, https://doi.org/10.1053/aq.1999.v19.102964001
Close - Share Icon Share
Abstract
Background: CO2 laser and erbium laser skin resurfacing techniques have gained considerable popularity in recent years. However, long-term results have demonstrated unexpected complications, including prolonged erythema and scarring. In response to these problems, many physicians have turned to systems, such as the combined CO2-erbium laser system, that seem to demonstrate fewer and less severe complications.
Objective: The purpose of this study was to evaluate the effectiveness of Visage Coblation, a new system for skin resurfacing that is based on bipolar electrocoagulation technology and was originally developed for use in arthroscopic surgery.
Methods: Twenty-three patients were treated with the Visage Coblation system from December 1998 to January 1999 using varying voltage and number of passes. Clinical results were evaluated postoperatively at 2 weeks and 1, 4, and 6 months. A histologic study was then performed on 4 samples of human tissue that had been treated with varying voltage and number of passes. The samples were harvested 2 hours after treatment so that the beginning of the inflammatory response in the surrounding tissues could be observed.
Results: Among the 23 patients treated in the clinical study, there were no major complications and recovery was relatively brief and comfortable. Aesthetic results were highly satisfactory in most patients, with improvement of fine and deep rhytids. The results demonstrated in the histologic study were similar to those seen with CO2-erbium laser systems, with complete exfoliation of the epidermis and a thin layer of coagulative collagen necrosis.
Conclusions: Although further investigation with longer-term follow-up is necessary, the Visage Coblation system may represent a new direction in the treatment of skin rejuvenation.
In recent years, there has been a growing interest in laser skin resurfacing. The CO2 laser demonstrated impressive results initially,1–4 but over time, it became apparent that the lengthy and uncomfortable postoperative period and frequent complications made this technique less attractive to many patients. Thermal damage to the treated tissue and a subsequent extended recovery period are the main problems resulting from use of the CO2 laser. The CO2 laser has a wavelength that is absorbed by intracellular water, causing tissue vaporization. The temperature that is reached causes thermal damage to the deep dermis. This problem is less marked with pulsed and ultrapulsed CO2 laser devices where the pulse is shorter than 1 ms, because the skin may cool between pulses.2,5,6 However, even with these devices, there is relatively severe thermal damage in the tissue around the target point, causing a prolonged reepithelization period of 7 to 14 days, marked serous exudation, and postoperative erythema that lasts 3 to 6 months.2,3 The thermal damage to the deep dermis is responsible for some postoperative complications such as scarring, hypopigmentation, hyperpigmentation, ectropion, and milia.2–4,6–10
Because moderate thermal necrosis stimulates collagen regeneration and produces good long-term aesthetic results in CO2 laser skin resurfacing, surgeons frequently try to improve results by increasing the power and the number of passes, thereby increasing the risk of complications.9
The erbium laser causes little thermal damage and involves a faster recovery, but the long-term results are not as good as those seen with the CO2 laser, because there is little collagen shrinkage and regeneration.8,11,12 Additionally, in the period immediately following erbium laser treatment there is uncomfortable bleeding in the treated area. The shortcomings of the CO2 laser and erbium laser systems have produced an interest in combined CO2-erbium laser technology and other alternatives.
The best resurfacing treatment would combine the epidermal exfoliation and thermal collagen necrosis in the superficial dermis that are attainable with the CO2 laser system and the short postoperative recovery period that is associated with erbium laser treatment. The combination CO2-erbium laser technology attempts to achieve this goal by using the erbium laser to cause exfoliation and a low-power CO2 laser to cause collagen shrinkage and regeneration with minimal thermal damage in the surrounding tissue.8 However, devices incorporating this combined technology are very expensive and increase surgical costs.
Visage Coblation (Arthrocare Corporation, Sunnyvale, CA), a new system that had been used previously in arthroscopic surgery, has demonstrated good results in cartilage removal and collagen shrinkage.
Mechanism of Action of the Visage Coblation System
Like other electrosurgical instruments, Visage Coblation establishes a high-frequency voltage between an electrode and the target tissue, creating an arc13,14 that seals the blood vessels and can ablate tissue by generating high temperatures. The size of the are depends on the size of the electrode and the applied voltage.
This new system is based on the technology that is used in conventional bipolar electrosurgical units. Unlike other electrosurgical units, the Visage Coblation system has 2 poles (electrodes) set very close to each other. An electrically conductive fluid (isotonic saline or Ringer's lactate solution) fills the physical gap between electrode and treated tissue.
When a sufficiently high voltage difference is applied between these structures, the fluid is converted into an ionized vapor layer (plasma) and the ions are accelerated toward the tissue with enough energy to dissociate the molecular bonds between the cells. This mechanism allows a volumetric removal of tissue that is confined to the surface layer and produces minimal thermal necrosis of the surrounding structures. The maximum temperature reached during the treatment is between 70° and 140°C, which is sufficient to cause collagen shrinkage and subsequent regeneration. Furthermore, if the voltage is reduced to a level at which the fluid cannot be transformed into plasma, small vessels can be coagulated to achieve a bloodless field.
The Visage Coblation system is a bipolar electrosurgical unit with a power range of 50 to 175 V. The unit is connected to a stylet whose electrodes are very close together, and the device allows a continous flow of saline solution. The results depend on the inclination of the stylet and the pressure applied on the skin, as well as on the voltage setting, which is easily controlled by a foot switch.
Materials and Methods
Clinical Methods
From December 1998 to January 1999, 23 patients with Fitzpatrick skin pigmentation types II and III underwent treatment with the Visage Coblation system. The patients were instructed to frequently apply creams containing glycolic acid 12% and hydroquinone 2% preoperatively for a period of 2 weeks. Beginning on the day before surgery, acyclovir (400 mg every 8 hours orally) and antibiotics (cephalexin 500 mg every 8 hours orally) were administered.
All procedures were performed either with local anesthesia with facial nerve blocks (lidocaine 2% with epinephrine 1:100,000) and infiltration (lidocaine 0.25% with epinephrine 1:100,000) or with intravenous sedation (midazolam, atropine, and fentanyl citrate), depending on the treated area.
The periocular area was treated in 15 patients, the perioral area was treated in 8 patients, and 3 patients underwent full-face resurfacing (Figure 1). The skin lesions treated included fine and deep rhytids, hyperkeratosis, and age spots.

A, C, E, G, Preoperative views of a 73-year-old woman. B, D, F, H, Postoperative views 8 months after full-face resurfacing with the Visage Coblation system. Two passes were made in the periorbital area and 4 passes in all other areas at maximum voltage (175 V). Note the improvement of fine and deep rhytids and the change in skin texture and color.
The voltage used (50 to 75 V) and the number of passes performed (2) in the first 2 patients were very conservative. In subsequent cases, the maximum voltage (175 V) was used and 2 to 4 passes were performed, depending on the treated area (2 passes in the periorbital area and 4 passes in all other areas).
Postoperatively, a cold semiocclusive dressing with epidermal growth factor gel was applied for the first 2 days; this was followed by an open treatment with petroleum jelly and cold epidermal growth factor gel (Heberfar S.L., Madrid, Spain). Antibiotics (cephalexin 500 mg every 8 hours orally) and acyclovir (400 mg every 8 hours orally) were given from the day before surgery until the fifth postoperative day.
Each patient was seen daily until complete reepithelization was achieved—usually between the third and fifth postoperative days. At that time, the patients were instructed to use moisturizing cream, sun protection,15 and makeup for hypersensitive skin to conceal erythema. Patients were seen for follow-up at 2 weeks, 1 month, 4 months, and 6 months postoperatively.
Histologic Methods
Histologic studies were performed using skin from the inferior left breast of a volunteer breast reduction patient. Four samples that had been treated with increasing voltage and number of passes were prepared, each 3 · 1.5 cm in size. Four specimens treated with the Visage Coblation system and 1 control specimen were harvested 2 hours after treatment.
Results
Clinical Results
Complete reepithelization was observed in all 23 patients within 5 days, and from that time forward, all were able to wear makeup for hypersensitive skin and return to normal daily activities (Figure 2).
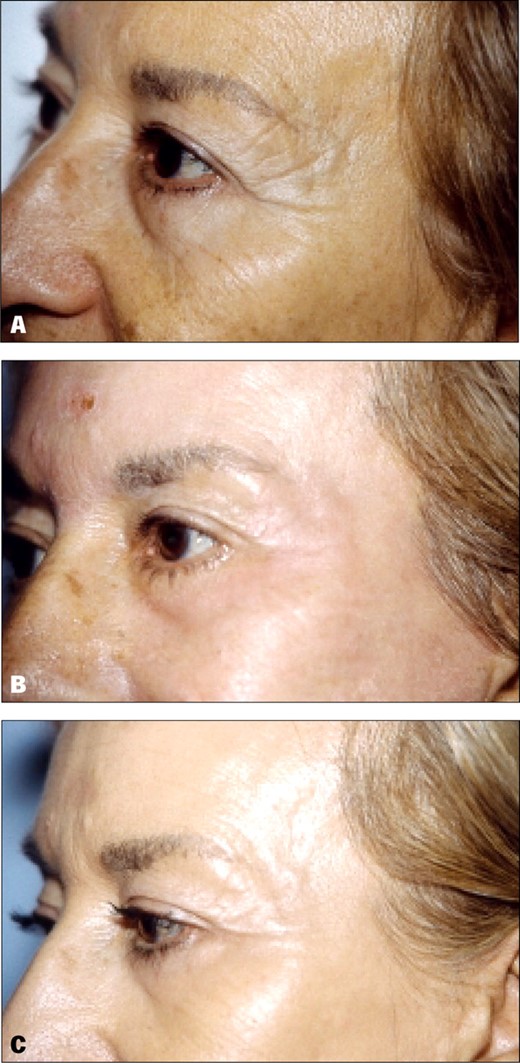
A, Preoperative view of a 63-year-old woman. B, Postoperative view 5 days after periorbital resurfacing with 2 passes at 175 V. Note the complete reepithelization with minimal swelling and erythema. C, Postoperative view at 6 months shows good improvement of crow's-feet lines.
Edema was common in the first 48 hours after treatment and was particularly marked in the periorbital area. The edema resolved spontaneously without treatment in every case. There were no complaints of postoperative pain or itching, and postoperative erythema was minimal, disappearing completely within 3 weeks.
Aesthetic results were very satisfactory in all patients except the initial two, who had received treatment with lower voltage. Significant improvement of fine and deep rhytids was seen. All skin discolorations disappeared (Figure 1). As with the CO2 laser, the results continued to improve over the next several months, suggesting collagen regeneration and deposition.1,2,8,16 One patient experienced extremely dry skin postoperatively, which required treatment for resolution. All patients stated that they would repeat the treatment.
Histologic Results
In the first sample, 2 passes were performed at 75 V. Total exfoliation of the epidermis was observed, with coagulative necrosis of the smaller superficial vessels and necrosis of the infundibular portion of the hair follicles. Infiltration of lymphocytes and histiocytes was also observed (Figure 3).
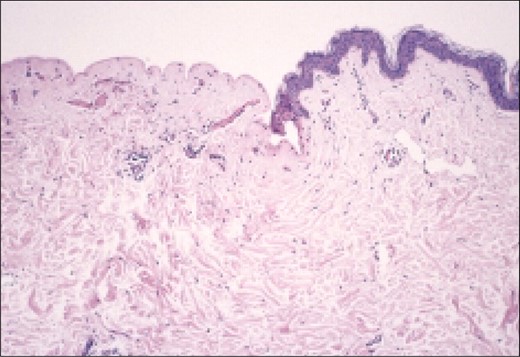
Photomicrograph of tissue treated with 2 passes at 75 V shows complete epidermal exfoliation.
In the second sample, 2 passes were performed at 125 V. The findings were similar to those seen in the first sample, with the addition of partial necrosis of the sweat ducts.
In the third sample, 2 passes were performed at 175 V. The findings were similar to those seen in the first and second samples, with the addition of a layer of coagulative collagen necrosis to a depth of 0.23 mm.
In the fourth sample, 4 passes were performed at 175 V. The effects seen in the 3 previous samples were observed, with an increase in the depth of collagen necrosis to 0.31 mm (Figure 4).
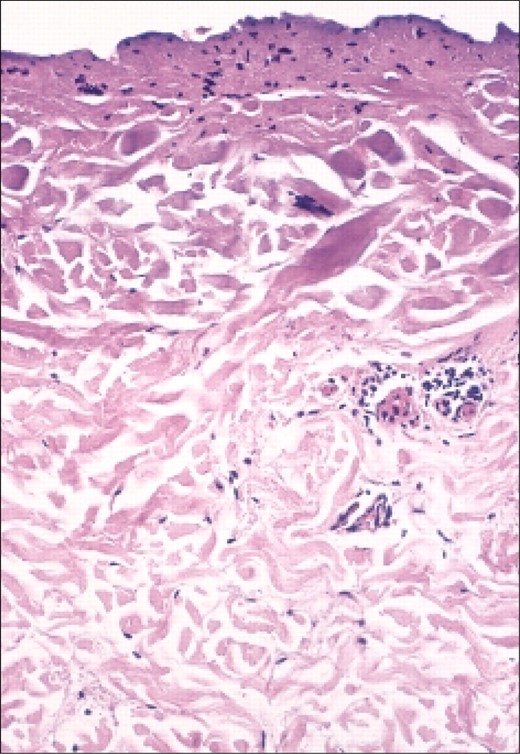
Photomicrograph of tissue treated with 4 passes at 175 V shows layer of thermal coagulative necrosis of the collagen.
In the control sample, the epidermis was 0.033 mm thick, and no histologic alterations were found.
These results are similar to those obtained with the CO2 laser11,17 and the CO2-erbium laser3 and demonstrate that 2 passes at a very low setting (sample 1) cause complete epidermal exfoliation. Furthermore, increasing the power results in collagen necrosis that can be controlled by the number of passes applied (samples 3 and 4). Therefore, the skin can be exfoliated with minimal and controlled thermal damage of the dermis.
Complications
In 2 cases, there was postoperative hyperpigmentation attributable to patient misunderstanding of the postoperative sunscreen recommendations; the condition was resolved by a 2-week course of hydroquinone topical cream. All postoperative erythema disappeared within 3 weeks, at which time patients were able to resume use of their normal makeup. There were no cases of hypertrophic scarring, hypopigmentation, milia, or infection. One patient's skin became extremely dry and required treatment with supplemental moisturizing cream for resolution.
Conclusions
Because of the small number of patients and the short postoperative period, the results presented here are not adequate to allow the development of solid conclusions about this new method for the treatment of aging skin. In this preliminary study, however, the Visage Coblation system shows promise as an alternative to the other methods of treatment currently in use. The histologic results are very similar to those seen with CO2-erbium laser treatment, and they are consistent with the clinical results. Advantages of this new system include a lower price for the equipment and faster, less painful treatment. The greatest advantage of the new system appears to be the reduction in temperature attained during the treatment process, which seems to prevent thermal damage to the surrounding tissue. As a result, complications such as the prolonged erythema and scarring that sometimes occur with the other systems are absent. The temperature reduction may also contribute to the shorter, less painful recovery period. The patient can return to normal activities approximately 1 week after the procedure.
The system requires precision for optimal use because the results are dependent not only on the voltage used and the number of passes performed but also on such factors as the amount of pressure applied during the treatment and the inclination of the stylet over the skin. The Visage Coblation system deserves further evaluation as a potential alternative for facial skin rejuvenation. Further investigation is necessary to define indications, protocol, and possible complications.
References
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
- arthroscopy
- epidermis
- cicatrix
- collagen
- erbium
- erythema
- esthetics
- follow-up
- lasers
- necrosis
- rejuvenation
- surgical procedures, operative
- carbon dioxide
- electrocoagulation
- skin
- surgery specialty
- peeling of skin
- carbon dioxide lasers
- dermabrasion with laser
- inflammatory response
- skin wrinkling
- skin resurfacing
- voltage



