-
PDF
- Split View
-
Views
-
Cite
Cite
Joseph W Glovacz, Sarah G Betts, Steven Cross, Justin Powell, Pharmacists’ impact on quality and financial metrics utilizing virtual care platforms during the coronavirus pandemic, American Journal of Health-System Pharmacy, Volume 79, Issue 11, 1 June 2022, Pages 904–908, https://doi.org/10.1093/ajhp/zxac044
Close - Share Icon Share
Abstract
Because of rising concern about coronavirus disease 2019 transmission, there has been a large shift from face-to-face, in-office visits to a virtual care model. The purpose of this article is to explain how Ascension Florida Gulf Coast was able to maximize the utility of ambulatory care pharmacists (ACPs) in the primary care setting during the pandemic and to provide guidance for creating a sustainable billing and practice model in the event of another global health crisis.
By employing telehealth services, our ACPs were able to continue to co-manage chronic disease states for documented diagnoses while still maintaining health-system revenue in the midst of a global health crisis. Utilizing various virtual platforms, ACPs were able to accommodate the needs of our patients while addressing concerns related to the compatibility and user friendliness of the platforms for our diverse patient population. ACPs used traditional incident-to evaluation and management services current procedural terminology billing codes with a virtual visit modifier for billing and tracking purposes.
Utilizing various virtual care platforms, our ACPs completed 447 patient encounters within the first 7 months of the pandemic. During this time, our ACPs addressed various population health metrics, specifically for patients diagnosed with diabetes without an active claim for a cholesterol-lowering medication, in addition to performing chronic disease management. Our ACPs had a 23% success rate for statin initiation in patients reviewed and contacted. By adopting virtual care options, our ACPs were able to effectively co-manage and educate patients while improving quality metrics and generating $50,662.24 in billable encounters for the health system during a global health crisis. The addition of ACP virtual encounters to primary care clinics both increases access to healthcare and improves patient care quality and outcomes while limiting revenue losses in our local health system.
Telehealth services enable ambulatory care pharmacists (ACPs) to manage chronic disease states in the setting of a global health crisis that requires physical distancing during a nationwide lockdown.
Because of limitations set by state-specific laws and emergency use authorizations, telehealth for ACPs may not be sustainable outside of a global health crisis.
In the event of a future pandemic, telehealth is a viable and potentially fiscally favorable option, as well as a quality improvement strategy, for a healthcare system.
Ambulatory care pharmacists (ACPs) are now considered to be vital assets to the healthcare team in various settings, so, when the World Health Organization declared the novel coronavirus 2019 (COVID-19) a global pandemic in March 2020, ACPs were forced to quickly develop a plan to improve the accessibility of their practices during a national lockdown. ACPs and their healthcare teams worked together to develop a plan that did not compromise patient outcomes or health-system revenues while still abiding by local and federal regulations as well as maintaining physical distancing to ensure the health and safety of patients and staff. The purpose of this article is to explain how Ascension Florida Gulf Coast was able to maximize the utility of ACPs in the primary care clinic setting during the novel COVID-19 era and to provide guidance for creating a sustainable billing and practice model in the event of another global health crisis.
Telehealth, also referred to as telemedicine, is defined as “the use of medical information exchanged from one site to another via electronic communications to improve a patient’s health status” by the American Telemedicine Association (ATA) and has been utilized for more than 30 years.1 There are multiple approaches to telehealth, including virtual visits, telephone communications, remote patient monitoring, and chat-based interaction via the Internet or mobile applications. These processes were originally established to expand physician care in rural areas where healthcare may be less accessible. Telehealth is used today by virtually all types of healthcare professionals and specialties for disease state management, medication therapy management, physician-to-physician consultations, and much more.2 Patients are able to interact with healthcare providers, including pharmacists, via video conference calls, electronic instant messaging, and wireless health monitoring devices. Accessibility to these modalities can vary depending on the availability of computers, tablets, landlines, and cell phones. Telehealth enables patients to talk with providers any time of day from anywhere in the world while potentially reducing healthcare costs for both the patient and health system. In new research, implementation of a virtual platform in the outpatient setting has been shown to reduce the spread of COVID-19 while ensuring that the high quality of patient encounters is maintained.3
Our single-center, multiclinic retrospective analysis was given exempt status by Ascension Florida Gulf Coast’s institutional review board based on the absence of patient risk and its retrospective nature.
Transitioning to a telehealth service
In Florida, despite executive order 20-91, otherwise known as the “Safer at Home” order, demands for healthcare did not slow: disease states outside of COVID-19 still existed and required management.4 In efforts to limit the number of people infected at any given time, or to “flatten the curve,” new, alternative methods for patient care had to provide physical distancing for the sake of staff and patient safety during a time of uncertainty related to outcomes and treatment for COVID-19. When developing new methods for delivering patient care, it is also important to ensure that the quality of care and patient outcomes are not compromised, in this case, by the physical distance between the provider and the patient. Finding a balance between these concerns in addition to the stress of maintaining health-system revenues during a pandemic did not allow much time for planning. Use of telehealth in the form of telephone appointments had been shown to be effective at other organizations, most notably in the Veterans Affairs Health System.5 Other documented uses of telehealth included virtual platforms for telehealth, which were utilized primarily by physicians in an attempt to provide healthcare to patients living in rural areas that do not have adequate or accessible healthcare opportunities.6
This paradigm shift for ACPs and patients provided a unique opportunity for potential growth and outreach. Implementation of telehealth enables more patients to attend appointments, whether from their home, their car, or work. Virtual platforms increase healthcare accessibility for patients, even for those who do not live in rural parts of the country. Our faith-based institution was one of the first to implement a strategy that combined virtual platforms providing real-time video conferencing with telephone calls. With this new delivery of patient care, ACPs were able to aid in overcoming the hurdles associated with physical distance and help provide a solution without additional cost or complexity for patients or our organization at large.
Telehealth care model
In the state of Florida, historically, ACPs have encountered challenges due to the lack of collaborative practice capabilities allowable under state pharmacy practice law. The global pandemic added yet another hurdle to overcome. With the help of our preexisting protocol, which allowed our ACPs to practice and co-manage disease states at the top of their licensure, ACPs were able to have both a clinical and personal impact through the implementation of a telehealth process that included virtual visits during the rise of the pandemic and throughout its course.
Clinic descriptions.
Our ACPs work in primary care and chronic disease management settings with physicians and midlevel providers. In these settings, the ACPs practice under a protocol established through the hospital’s pharmacy and therapeutics committee as well as the medical group’s executive leadership council to co-manage chronic disease states for documented diagnoses including, but not limited to, diabetes, hypertension, hyperlipidemia, chronic obstructive pulmonary disease, hypothyroidism, osteoporosis, anemia, mood disorders, and chronic heart failure.
Before the pandemic, the ACPs had an average of 7 in-person appointments per day. As the COVID-19 pandemic escalated in the United States, the number of in-person office visits substantially decreased. Until a permanent solution could be achieved, telephone appointments were utilized to avoid lapses in patient care. This came at a cost to the medical group due to the inability of ACPs to bill insurance for any appointments carried out over the telephone. Despite this shortcoming, patient care was the ultimate priority, and telephone appointments conducted by ACPs were successfully used to bridge the gap from in-person visits to virtual visits.
ACPs capitalized on additional avenues to close patient care gaps established by Medicare. With the “Safer at Home” executive order in place, the likelihood of ACPs successfully contacting patients by telephone improved. Our clinic focused primarily on reaching out to patients with a diagnosis of diabetes who were not currently on a statin. To close this care gap, the ACPs and their team utilized both postgraduate year 1 and postgraduate year 2 pharmacy residents to contact patients between appointments who were flagged by their insurance as having this care gap to discuss initiation of statin therapy. If the patient agreed to therapy, our clinic had an established protocol in place that allowed the ACPs to place an order for an appropriate statin as well as set up a follow-up visit with their primary care provider. If the patient declined initiation of therapy, this was documented in their chart.
Telehealth technology.
During the transition period from telephone appointments to virtual platforms with video conferencing capabilities, our ACPs used a trial-and-error approach when selecting a platform that met both staff and patient needs. There was a rapid transition to virtual platforms, including Amwell (Amwell, Boston, MA), Doximity (Doximity, San Francisco, CA), and Google Meets (Google, Mountain View, CA), with the majority opting for Doximity given that access to smartphones is nearly universal and no additional software applications were required. A few important factors that were considered when selecting a virtual platform for patient care included the ability to maintain patient privacy, the complexity of use, the accessibility for patients, and the cost to the medical group. The virtual platform also had to be able to accommodate the needs of a diverse patient population, including patients who might not have access to a smartphone.
Billing model.
When integrating virtual telehealth appointments into the clinic, development of a billing model for appointments was a crucial next step of the process. Because of Florida’s state laws and pharmacists’ lack of provider status in the state, ACPs are restricted in the services they may perform and how they are able to bill for these services. Ascension Florida Gulf Coast currently utilizes a billing model based on appointment duration. Virtual telehealth appointments were billed using the standard evaluation and management services Current Procedural Terminology (CPT) codes previously used for in-person encounters. A virtual visit modifier, VV, was appended to each standard code, but the codes had the same reimbursement rates as for inpatient encounters. CPT billing codes 99211,VV through 99215,VV were used for virtual appointments. For short, minimal-complexity appointments lasting around 5 minutes, the 99211,VV code was used. In the event that a virtual appointment was attempted but all attempts at real-time, face-to-face interaction were unsuccessful owing to Internet connectivity issues or user error, a telephone appointment was used instead and billed for as a virtual visit using the above codes.
All telephone appointments, including those for statin use in patients with diabetes, were billed for encounter tracking purposes only as 98966-8,A, as patients were contacted for quality purposes.
Impact of the program
Use of telehealth with ACPs in the primary care setting during the global COVID-19 pandemic increased patient accessibility to healthcare services while maintaining physical distancing for safety, thereby not compromising patient care or causing significant loss of medical group revenue. From March 2, 2020, to October 30, 2020, our ACPs billed for 99211,VV encounters 22 times at $36.30 per encounter. For encounters lasting 10 minutes with established patients, code 99212,VV was billed. The reimbursement rate for these claims is $91.02 per encounter, and this code was billed 63 times during the prespecified time frame. Most appointments during the pandemic were billed using the 99213,VV code, which was applied for 15-minute appointments with established patients. We billed $170.98 each for 205 such encounters. More complex established patients were billed with code 99214,VV or 99215,VV depending on the duration of the appointment. Appointments lasting 25 minutes were billed for $252.18 with code 99214,VV, which was documented 36 times. Lastly, any appointment lasting 40 minutes or longer was billed with code 99215,VV for $371.30 per encounter. During the prespecified time frame, no appointments were billed with 99215,VV (Figure 1). In sum, the encounters provided an estimated reimbursement of $50,662.24 over 7 months (Figure 2), indicating that the billing model for virtual telehealth utilizing ACPs is sustainable in the setting of a global health crisis. In addition, ACPs capitalized on patients being at home because of the pandemic to successfully reach out to patients via telephone to discuss options to optimize their health plan, ultimately closing a number of gaps in care identified.
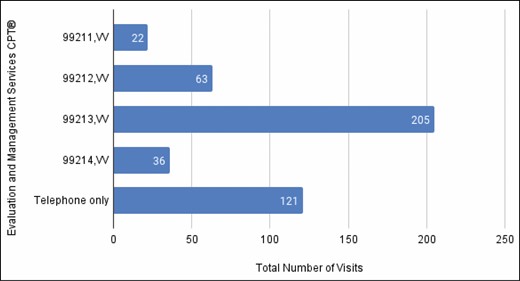
Total number of visits (March to October 2020). CPT indicates Current Procedural Terminology.
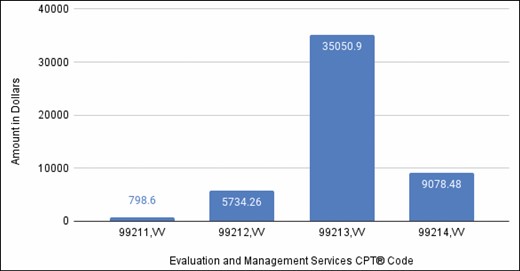
Total amount billed by CPT code. CPT indicates Current Procedural Terminology.
For quality calls regarding statin use in patients with diabetes, our ACPs attempted 85 calls to patients, contacting 62. Of these 62 patients, 14 (22.6%) were initiated on statin therapy, closing a quality gap and potentially helping to decrease overall risk for stroke and heart attack in this patient population. These calls combined with telephone-only visits accounted for 121 total patient encounters from March to October 2020 (Figure 3).
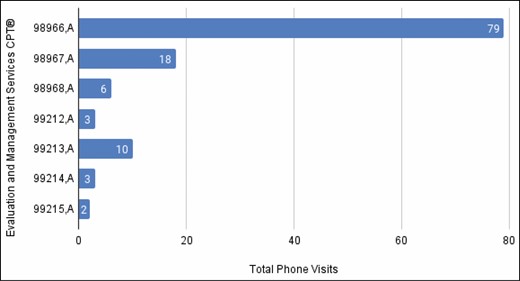
Telephone visits by CPT code. CPT indicates Current Procedural Terminology.
Furthermore, the longstanding need for pharmacists in the primary care setting is further reinforced in the context of an overburdened healthcare system that currently has limited capacity for patient contact and a continued need for chronic disease management. Utilizing various virtual care platforms, our ACPs completed 447 patient encounters within the first 7 months of the pandemic. Based on the average daily patient volume, our ACPs were able to recapture approximately 50% of clinic volume from before the pandemic. This average may have been skewed due to initially low clinic volume at the start of the pandemic. However, toward the end of our data collection period, clinic volume numbers were approaching 75% or more of the volume before the pandemic as telehealth technology was better understood and accepted by our patients. By adopting and embracing virtual care options, our ACPs were able to effectively teach, coach, and educate patients while improving multiple quality metrics and generating billable encounters (amounting to approximately $50,000) for the health system. While care and payment models that pivoted during the global pandemic may return to previous models after the crisis ends, leaders may consider this care model as an opportunity given the likelihood of another pandemic. The addition of ACP virtual encounters to primary care clinics has both increased access to healthcare and improved patient care, while limiting loss of revenue within our local health system, during the ongoing global pandemic.
Conclusion
In summation, our ACPs were able to utilize virtual care platforms to enhance patient care by increasing availability to a provider and addressing acute and chronic issues with patients in real time without sacrificing potential income to our organization. The findings in this paper demonstrate not only the value ACPs provide to patients, but also the potential patient care and financial value of ACPs to providers and the organization at large.
This article is part of a special AJHP theme issue on telehealth. Contributions to this issue were coordinated by Michael J. Miller, BSPharm, DrPH, FAPhA; Sandra L. Kane-Gill, PharmD, MS, FCCM, FCCP; and Hae Mi Choe, PharmD.
Disclosures
The authors have declared no potential conflicts of interest.




Comments