-
Views
-
Cite
Cite
Edward R Horton, Bryce V Johnson, Mahesh Vidula, Jonathan J Lee, Soumya Kondaveeti, Caroline A Magro, Srivinas Denduluri, Patrick Segers, Howard C Herrmann, Julio A Chirinos, Arterial Properties and Ventricular–Arterial Interactions in Severe Aortic Stenosis: Impact on Prognosis, American Journal of Hypertension, Volume 38, Issue 5, May 2025, Pages 321–330, https://doi.org/10.1093/ajh/hpae127
Close - Share Icon Share
Abstract
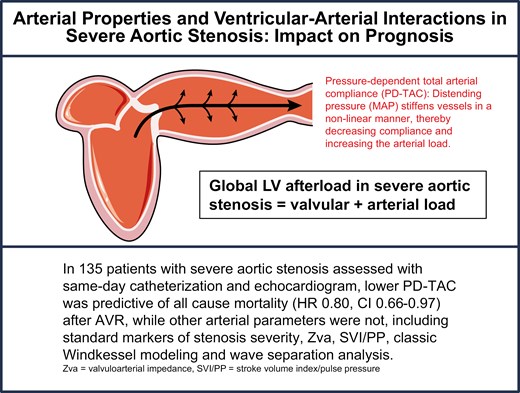
Systemic arterial properties contribute to clinical heterogeneity and outcomes in degenerative calcific aortic stenosis (AS). Lumped parameters of afterload have previously been associated with adverse left ventricular remodeling, mortality, and poor exercise tolerance in this population, but most studies did not assess pulsatile aortic pressure–flow relations, the gold standard method for assessing arterial load. Moreover, arterial compliance is highly dependent on nonpulsatile (mean) arterial pressure, which influences prognosis in this population.
We retrospectively studied 135 patients with severe AS with same-day catheterization and echocardiogram. Invasive aortic pressures and echocardiographic flow waveforms were used to assess pressure–flow and pressure–volume relations using Windkessel modeling and wave separation analyses. We used Cox regression to assess the relationship between pulsatile load and time to death and heart failure hospital admission (DHFA).
Total arterial compliance accounting for pressure dependence was independently predictive of all-cause mortality (Hazard Ratio (HR) = 0.80, 95% confidence interval [CI] = 0.66–0.97; P = 0.023) and DHFA (HR = 0.70; 95% CI = 0.50–0.97; P = 0.031) even after adjustment for age, race, gender, body mass index, and comorbidities, whereas other arterial parameters were not.
In patients with severe AS, pressure-dependent arterial compliance predicts adverse outcomes, whereas traditional pulsatile arterial load measures do not. Our findings suggest that methods accounting for pressure load on the arterial wall are advantageous in this population in which lower mean pressure can result from severe stenosis and ventricular dysfunction.