-
PDF
- Split View
-
Views
-
Cite
Cite
Brendan J Belovarac, Sondra R Zabar, Dana Warfield, Michael A Bannan, Amy V Rapkiewicz, The OSPE: Objective Structured Pathology Examination, American Journal of Clinical Pathology, Volume 155, Issue 3, March 2021, Pages 324–332, https://doi.org/10.1093/ajcp/aqaa143
Close - Share Icon Share
Abstract
Resident assessment tends to consist of multiple-choice examinations, even in nuanced areas, such as quality assurance. Internal medicine and many other specialties use objective structured clinical examinations, or OSCEs, to evaluate residents. We adapted the OSCE for pathology, termed the Objective Structured Pathology Examination (OSPE).
The OSPE was used to evaluate first- and second-year residents over 2 years. The simulation included an anatomic pathology sign-out session, where the resident could be evaluated on diagnostic skills and knowledge of key information for cancer staging reports, as well as simulated frozen-section analysis, where the resident could be evaluated on communication skills with a “surgeon.” The OSPE also included smaller cases with challenging quality issues, such as mismatched slides or gross description irregularities. All cases were scored based on the Pathology Milestones created by the Accreditation Council for Graduate Medical Education.
Using this OSPE, we were able to demonstrate that simulated experiences can be an appropriate tool for standardized evaluation of pathology residents.
Yearly evaluation using the OSPE could be used to track the progress of both individual residents and the residency program as a whole, identifying problem areas for which further educational content can be developed.
Simulated encounters, such as those frequently used by more patient-facing specialties, can be adapted to the specific needs of a pathology residency program.
This feasibility study described the Objective Structured Pathology Examination (OSPE), which can provide pathology residency programs an alternative method for assessing pathology residents and identifying areas for improvement.
The OSPE also provides a method to assess residents within the Accreditation Council for Graduate Medical Education milestone framework that is more objective and less dependent on factors such as rotation timing than traditional faculty evaluations.
The approach to assessment of residents and programmatic evaluation of pathology training programs has dramatically changed over the past decade. Competency-based education and evaluation were formally introduced into graduate medical education in 1998 via the Outcome project by the Accreditation Council for Graduate Medical Education (ACGME). In 2013, the ACGME began implementation of the Next Accreditation System (NAS).1 While the emphasis on the six core competencies2,3 remains, the system also aims to institute metrics in graduate training programs based on resident achievement of specialty-specific milestones. The NAS also gives programs a larger role in continuous self-assessment, which puts a greater emphasis on assessment and evaluation of residents. In July 2015, the ACGME, in collaboration with the American Board of Pathology, released the Pathology Milestone Project. This collection of 27 categories, ranked on a scale from 0 to 5, is designed to evaluate the six core competencies as they relate to pathology,4 with a recommendation that they be reviewed during residents’ semiannual evaluations. These milestones have recently been updated and simplified, with the 2019 Pathology Milestones rolled out in the 2019-2020 academic year. Individual institutions are tasked with developing their own methods of evaluating residents using these milestones. The ACGME further introduced the Clinical Learning Environment Review (CLER) program in 2012 to provide feedback to graduate medical education (GME) programs related to six areas of patient care, including aspects such as professionalism and patient safety.5 At our institution, we have piloted the implementation of objective structured clinical examinations (OSCEs) as a method for resident evaluation as relating to many aspects of the ACGME milestones, and thus core competencies and the CLER focus on areas that are relevant to pathology training.
Performance-based assessments or OSCEs have been a mainstay in undergraduate medical education, particularly in the evaluation and assessment of clinical skills as they relate to the continuum of training.6-8 In addition, residencies in areas such as internal medicine have adapted these evaluations to their programs as a way of formally tracking resident progress.9,10 While milestones have been clearly delineated by the ACGME, pathology residency programs are also in need of tools that can be used to objectively evaluate resident performance. Most OSCEs have been developed to assess patient interactions and clinical decision making, and to our knowledge OSCEs have not been implemented in pathology residency programs as a means of assessment. Instead, some programs predominately focus on direct observation during normal residency workflow, which will fall short of truly evaluating a resident’s competence in practice.11 Simulation is ideally used to demonstrate the developmental progression for common situations and offer opportunities to experience uncommon situations not readily encountered. These objective assessments using behavioral anchored checklists can also identify areas of weakness hidden from routine rote subjective evaluations, particularly those that deal with communication, interprofessional interactions, and systems practice.
With that in mind, we set out to develop a proof of concept for an Objective Structured Pathology Examination (OSPE), with one portion focused on quality assurance. We hoped to identify those residents who had not yet developed a practical understanding of the types of quality issues faced in the surgical pathology department, as well as those with specific areas for improvement with regard to communication skills and professionalism. The open-endedness of this experience helped to facilitate resident assessment in these areas.
Materials and Methods
Participants
The OSPE was given to all postgraduate year (PGY) 1 and PGY-2 anatomic pathology (AP) or AP/clinical pathology (CP) residents within a university residency program. The OSPE was given in 2 consecutive years. The purpose and a general overview of the OSPE were explained to the residents but not the specific topics that would be covered. The residents were told that the OSPE would be considered a part of their mandatory biannual evaluation process, but they could opt out of the OSPE and instead discuss with the residency director. During this time, 21 total residents participated; eight of the residents participated as PGY-1 level in the first year and as PGY-2 the following year, thus taking the OSPE twice. As our program is more AP focused during the first 2 years of residency education, we hoped that the OSPE would allow us to assess if by PGY-2 residents had a good understanding of the AP-focused topics in the OSPE. The residents were all enrolled in the GME research registry that was approved by the institutional review board at the institution.
OSPE Content and Format
A team consisting of four attending surgical pathologists developed a Simulation Examination Blueprint, which was carried out over 2 years. The OSPE consisted of both simulated interactions as well as the evaluation of surgical pathology cases. The simulated interactions were developed with the idea of being authentic to daily clinical practice within an AP service. Table 1 contains the instructions and materials provided to the residents prior to the simulated encounters for reference; the overview and script provided to the evaluator are shown in Table 2.
| Characteristic . | First—Sign-out With Junior Resident . | Second—Unexpected Malignancy on Frozen Section . | Third—Discussion of Risk and Frozen Sections . |
|---|---|---|---|
| Case scenario provided | The patient is a 60-year-old woman who underwent a screening colonoscopy, which revealed a right-sided mass, likely malignant. The lesion was biopsied and signed out as adenocarcinoma. The patient has a prior diagnosis of breast cancer and has undergone a lumpectomy with adjuvant chemotherapy. She underwent a partial colectomy. | The patient is a 61-year-old woman who is being followed for her borderline hypercalcemia. She presents to the ENT surgeon for a neck lipoma that has grown slowly over the years. Radiologic studies of the posterior neck mass appear benign. The workup of her hypercalcemia reveals increased uptake on technicium studies extending posteriorly from the lower pole of the right thyroid. It was interpreted as one abnormal parathyroid lesion. The patient was scheduled for lipoma removal and parathyroid excision. The patient had an FNA of the thyroid 2 years ago that was diagnosed as a colloid nodule. The surgeon sent down a prelaryngeal lymph node and parathyroid glands. The “parathyroid glands” weigh 0.4 g and 0.3 g. | The patient is a 56-year-old woman who saw her gynecologist for a routine annual examination. The doctor palpated a right adnexal mass and thought it was an ovarian cyst. A transvaginal ultrasound was performed and showed a complex right ovarian cyst. She was then sent to a gynecologic oncologic surgeon for evaluation. A surgery was scheduled. |
| Instructions given to the assessed resident | You are a senior resident looking at colon specimens today and signing out this case with a “junior resident,” played by an attending. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. |
| Simulation assignment | Make a written diagnosis on the slides provided to you. This diagnosis would be expected to look as a typical surgical pathology report with all of the expected requirements. Answer any questions the junior resident may have for you regarding the specimen. Discuss your plan for next steps regarding this specimen with the junior resident and what you may need from him or her. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions they may have. Discuss your follow-up plan for the pathology specimens with the surgeon. Follow through with the attending via a telephone call with your plan. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions the surgeon may have. Discuss your follow-up plan for the pathology specimens with the surgeon. |
| Characteristic . | First—Sign-out With Junior Resident . | Second—Unexpected Malignancy on Frozen Section . | Third—Discussion of Risk and Frozen Sections . |
|---|---|---|---|
| Case scenario provided | The patient is a 60-year-old woman who underwent a screening colonoscopy, which revealed a right-sided mass, likely malignant. The lesion was biopsied and signed out as adenocarcinoma. The patient has a prior diagnosis of breast cancer and has undergone a lumpectomy with adjuvant chemotherapy. She underwent a partial colectomy. | The patient is a 61-year-old woman who is being followed for her borderline hypercalcemia. She presents to the ENT surgeon for a neck lipoma that has grown slowly over the years. Radiologic studies of the posterior neck mass appear benign. The workup of her hypercalcemia reveals increased uptake on technicium studies extending posteriorly from the lower pole of the right thyroid. It was interpreted as one abnormal parathyroid lesion. The patient was scheduled for lipoma removal and parathyroid excision. The patient had an FNA of the thyroid 2 years ago that was diagnosed as a colloid nodule. The surgeon sent down a prelaryngeal lymph node and parathyroid glands. The “parathyroid glands” weigh 0.4 g and 0.3 g. | The patient is a 56-year-old woman who saw her gynecologist for a routine annual examination. The doctor palpated a right adnexal mass and thought it was an ovarian cyst. A transvaginal ultrasound was performed and showed a complex right ovarian cyst. She was then sent to a gynecologic oncologic surgeon for evaluation. A surgery was scheduled. |
| Instructions given to the assessed resident | You are a senior resident looking at colon specimens today and signing out this case with a “junior resident,” played by an attending. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. |
| Simulation assignment | Make a written diagnosis on the slides provided to you. This diagnosis would be expected to look as a typical surgical pathology report with all of the expected requirements. Answer any questions the junior resident may have for you regarding the specimen. Discuss your plan for next steps regarding this specimen with the junior resident and what you may need from him or her. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions they may have. Discuss your follow-up plan for the pathology specimens with the surgeon. Follow through with the attending via a telephone call with your plan. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions the surgeon may have. Discuss your follow-up plan for the pathology specimens with the surgeon. |
ENT, ear, nose, and throat; FNA, fine-needle aspiration.
| Characteristic . | First—Sign-out With Junior Resident . | Second—Unexpected Malignancy on Frozen Section . | Third—Discussion of Risk and Frozen Sections . |
|---|---|---|---|
| Case scenario provided | The patient is a 60-year-old woman who underwent a screening colonoscopy, which revealed a right-sided mass, likely malignant. The lesion was biopsied and signed out as adenocarcinoma. The patient has a prior diagnosis of breast cancer and has undergone a lumpectomy with adjuvant chemotherapy. She underwent a partial colectomy. | The patient is a 61-year-old woman who is being followed for her borderline hypercalcemia. She presents to the ENT surgeon for a neck lipoma that has grown slowly over the years. Radiologic studies of the posterior neck mass appear benign. The workup of her hypercalcemia reveals increased uptake on technicium studies extending posteriorly from the lower pole of the right thyroid. It was interpreted as one abnormal parathyroid lesion. The patient was scheduled for lipoma removal and parathyroid excision. The patient had an FNA of the thyroid 2 years ago that was diagnosed as a colloid nodule. The surgeon sent down a prelaryngeal lymph node and parathyroid glands. The “parathyroid glands” weigh 0.4 g and 0.3 g. | The patient is a 56-year-old woman who saw her gynecologist for a routine annual examination. The doctor palpated a right adnexal mass and thought it was an ovarian cyst. A transvaginal ultrasound was performed and showed a complex right ovarian cyst. She was then sent to a gynecologic oncologic surgeon for evaluation. A surgery was scheduled. |
| Instructions given to the assessed resident | You are a senior resident looking at colon specimens today and signing out this case with a “junior resident,” played by an attending. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. |
| Simulation assignment | Make a written diagnosis on the slides provided to you. This diagnosis would be expected to look as a typical surgical pathology report with all of the expected requirements. Answer any questions the junior resident may have for you regarding the specimen. Discuss your plan for next steps regarding this specimen with the junior resident and what you may need from him or her. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions they may have. Discuss your follow-up plan for the pathology specimens with the surgeon. Follow through with the attending via a telephone call with your plan. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions the surgeon may have. Discuss your follow-up plan for the pathology specimens with the surgeon. |
| Characteristic . | First—Sign-out With Junior Resident . | Second—Unexpected Malignancy on Frozen Section . | Third—Discussion of Risk and Frozen Sections . |
|---|---|---|---|
| Case scenario provided | The patient is a 60-year-old woman who underwent a screening colonoscopy, which revealed a right-sided mass, likely malignant. The lesion was biopsied and signed out as adenocarcinoma. The patient has a prior diagnosis of breast cancer and has undergone a lumpectomy with adjuvant chemotherapy. She underwent a partial colectomy. | The patient is a 61-year-old woman who is being followed for her borderline hypercalcemia. She presents to the ENT surgeon for a neck lipoma that has grown slowly over the years. Radiologic studies of the posterior neck mass appear benign. The workup of her hypercalcemia reveals increased uptake on technicium studies extending posteriorly from the lower pole of the right thyroid. It was interpreted as one abnormal parathyroid lesion. The patient was scheduled for lipoma removal and parathyroid excision. The patient had an FNA of the thyroid 2 years ago that was diagnosed as a colloid nodule. The surgeon sent down a prelaryngeal lymph node and parathyroid glands. The “parathyroid glands” weigh 0.4 g and 0.3 g. | The patient is a 56-year-old woman who saw her gynecologist for a routine annual examination. The doctor palpated a right adnexal mass and thought it was an ovarian cyst. A transvaginal ultrasound was performed and showed a complex right ovarian cyst. She was then sent to a gynecologic oncologic surgeon for evaluation. A surgery was scheduled. |
| Instructions given to the assessed resident | You are a senior resident looking at colon specimens today and signing out this case with a “junior resident,” played by an attending. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. | You are a resident pathologist on frozen-section rotation responsible for interpretation of the frozen-section slides made available. The “surgeon” has broken scrub and is sitting with you at the microscope. |
| Simulation assignment | Make a written diagnosis on the slides provided to you. This diagnosis would be expected to look as a typical surgical pathology report with all of the expected requirements. Answer any questions the junior resident may have for you regarding the specimen. Discuss your plan for next steps regarding this specimen with the junior resident and what you may need from him or her. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions they may have. Discuss your follow-up plan for the pathology specimens with the surgeon. Follow through with the attending via a telephone call with your plan. | Make a diagnosis on the frozen-section specimens and convey the diagnosis to the surgeon. You do not need to write anything down on paper. Answer any questions the surgeon may have. Discuss your follow-up plan for the pathology specimens with the surgeon. |
ENT, ear, nose, and throat; FNA, fine-needle aspiration.
| First Simulation . | Second Simulation . | This Simulation . |
|---|---|---|
| When the resident taking the OSPE enters the room, you, the “junior resident,” are sitting at the microscope waiting for them to begin looking at the slides. You introduce yourself as the “junior resident” and say we have a colon cancer case to look at and hand the slides over with a printed version of the report. If the resident does not ask to look at the gross description or images, ask the resident if they would like to see pictures of the gross. Describe the tumor location in the ascending colon and features (ulcerated mucosa with rolled edges). If the resident does not read the gross description at this time, tell them you were not sure how to describe it and ask if they can check over your gross description. The first two slides are margin slides; explain that you took these as a margin and ask if the lesion was closer, how you might have taken the margins. The next three slides are from the tumor. You let the senior resident look over the slides for 5 minutes or so. Following this time, you tell them that you thought this was a poorly differentiated tumor. Hopefully, they will correct you that this is a well to moderately differentiated tumor, but if not, ask for how you evaluate tumor differentiation. The items you are looking for the resident to discuss are: a. Depth of invasion: this tumor extends to and perforates the peritoneum. Tell the resident the only other colon cancer you grossed was a rectal cancer, and you remember the mesorectum being important. They should be able to discuss the evaluation of the mesorectum completeness. b. Margin status: the tumor is within 1 cm from the radial margin. Ask the resident what the radial margin is, as you read it in the books you were reading. c. Lymphovascular and perineural invasion | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You comment on how fast the pathology assistant grossed and prepared the frozen section. You then start out by saying, “So my parathyroid is 0.4 g, what do you think of that, Dr. X?” in a jovial way. If the resident does not acknowledge that this is enlarged, follow up the statement with, “Do you think that qualifies for adenoma?” Then ask the resident if they can look at the parathyroid first before the prelaryngeal node as you are so curious to see it. Ask the resident if the parathyroid is cellular and if it is consistent with an adenoma. The resident may inquire about intraoperative PTH levels and respond that they decreased following removal of the lesion. | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You mention that you thought this would be an easy case, but the cyst looked a little suspicious. Allow the resident around 5 minutes to evaluate the slides, then ask for the diagnosis. If the resident incorrectly identifies this borderline serous tumor as a more benign lesion, you may lead them toward the correct diagnosis by asking about the patterns you see (“Is this some kind of papillary thing? What’s that purple stuff?”). If they incorrectly call it a serous carcinoma, you may ask them to point out the invasion for you. Once you have gotten to the diagnosis, say, “I’m a little confused. Is this malignant, or not? Do I need to take more out?” The resident should be able to discuss with you the risk of serous borderline tumor, including the risk of recurrence and small possibility of development of serous carcinoma in the future. If the resident brings up the possibility of peritoneal implants or biopsies, you may state that you will consider this back in the operating room. |
| After the resident looks at all the slides, see if they comment on the number of lymph nodes (4). If they do not, say that when you grossed the specimen, you only found four lymph nodes. Hopefully, they will tell you the requirements needed for lymph node sampling and that you need to go back and sample more lymph nodes. | Next ask the resident to look at the lymph node. Inform the resident that it is your process to remove the lymph node if it appears prominent during surgery. If the resident correctly identifies metastatic thyroid carcinoma within the node, act surprised. Ask the resident if they are sure and to explain to you why they think it is thyroid carcinoma. Ask the resident if it could be heterotopic thyroid tissue. Inform the resident that you will be sending the thyroid gland shortly. If the resident does not identify the carcinoma, tell them you were concerned because you know the patient had a thyroid mass in the past and you see it now during the procedure. See if the resident rescans the slide to double check their work. If not, tell them you may be sending a hemithyroidectomy and that you would hate to have to go back to operate as this patient is very anxious about any procedure. If they are still confident that the node is negative, ask them to look at the last case. | Next ask the resident if there are some “stains” that could be done to prove if this is “malignant or not.” The resident should explain to you that this diagnosis does not depend on staining but rather on histologic features and the absence of invasion. |
| Tell the “senior resident” you have a silly question: how would I know this is not metastatic breast carcinoma? Hopefully, the “senior resident” will explain that in many cases of colorectal cancer, you can see a precursor dysplastic lesion and that it is unlikely for breast cancer to metastasize to the colon. Ask if there are any immunohistochemical stains that you could use to distinguish breast from colorectal carcinoma. You are looking for the resident to answer CK7, CK20, and other markers such as GATA-3, ER, and PR. Finally, you will want to discuss microsatellite instability testing, BRAF, and Kras testing. The resident will relay a plan for follow-up on the case and explain a practice on how to resample for lymph nodes. If prompted about lymph nodes, you will tell the “senior resident” that your plan is to regross the fat to look for lymph nodes and ask if there are any stains or things that you want done for the case. If they ask about the synoptic worksheet, ask how you fill out the synoptic worksheet and hand it to them. When they get to microsatellite instability and molecular testing, ask them why you need to do this. Finish up by saying you will order blank stains for molecular studies. | The resident will look at the remaining “parathyroid” frozen section. Tell them you saw this and thought it was another parathyroid gland or lymph node. If the resident identifies the tissue as parathyroid, act surprised and say that your error rate for gross prediction of parathyroid vs lymph node is very poor. If they identify the tissue as lymph node and seem confident and satisfied, tell them that you are going to close and discuss a hemithyroidectomy with the patient after she heals from this procedure and repeats another FNA. During this encounter, ask the resident to tell you why they think it is a lymph node. If the resident identifies the tissue as thymus, seem interested and ask the resident to explain to you why they think it is thymus. End the encounter by thanking them and ask them to give you a synopsis of what the diagnoses are, then leave the room. | Finally, mention to the resident that the cyst was a lot larger than what you see on the slides, and ask if they should process more tissue for frozen diagnosis. If the resident asks, say it was at least 10 cm. The resident should be able to discuss how selected areas are chosen for frozen-section diagnosis and the limitations of frozen sections for larger specimens. Finish by thanking the resident and asking for a summary of the findings and their recommendations. |
| First Simulation . | Second Simulation . | This Simulation . |
|---|---|---|
| When the resident taking the OSPE enters the room, you, the “junior resident,” are sitting at the microscope waiting for them to begin looking at the slides. You introduce yourself as the “junior resident” and say we have a colon cancer case to look at and hand the slides over with a printed version of the report. If the resident does not ask to look at the gross description or images, ask the resident if they would like to see pictures of the gross. Describe the tumor location in the ascending colon and features (ulcerated mucosa with rolled edges). If the resident does not read the gross description at this time, tell them you were not sure how to describe it and ask if they can check over your gross description. The first two slides are margin slides; explain that you took these as a margin and ask if the lesion was closer, how you might have taken the margins. The next three slides are from the tumor. You let the senior resident look over the slides for 5 minutes or so. Following this time, you tell them that you thought this was a poorly differentiated tumor. Hopefully, they will correct you that this is a well to moderately differentiated tumor, but if not, ask for how you evaluate tumor differentiation. The items you are looking for the resident to discuss are: a. Depth of invasion: this tumor extends to and perforates the peritoneum. Tell the resident the only other colon cancer you grossed was a rectal cancer, and you remember the mesorectum being important. They should be able to discuss the evaluation of the mesorectum completeness. b. Margin status: the tumor is within 1 cm from the radial margin. Ask the resident what the radial margin is, as you read it in the books you were reading. c. Lymphovascular and perineural invasion | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You comment on how fast the pathology assistant grossed and prepared the frozen section. You then start out by saying, “So my parathyroid is 0.4 g, what do you think of that, Dr. X?” in a jovial way. If the resident does not acknowledge that this is enlarged, follow up the statement with, “Do you think that qualifies for adenoma?” Then ask the resident if they can look at the parathyroid first before the prelaryngeal node as you are so curious to see it. Ask the resident if the parathyroid is cellular and if it is consistent with an adenoma. The resident may inquire about intraoperative PTH levels and respond that they decreased following removal of the lesion. | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You mention that you thought this would be an easy case, but the cyst looked a little suspicious. Allow the resident around 5 minutes to evaluate the slides, then ask for the diagnosis. If the resident incorrectly identifies this borderline serous tumor as a more benign lesion, you may lead them toward the correct diagnosis by asking about the patterns you see (“Is this some kind of papillary thing? What’s that purple stuff?”). If they incorrectly call it a serous carcinoma, you may ask them to point out the invasion for you. Once you have gotten to the diagnosis, say, “I’m a little confused. Is this malignant, or not? Do I need to take more out?” The resident should be able to discuss with you the risk of serous borderline tumor, including the risk of recurrence and small possibility of development of serous carcinoma in the future. If the resident brings up the possibility of peritoneal implants or biopsies, you may state that you will consider this back in the operating room. |
| After the resident looks at all the slides, see if they comment on the number of lymph nodes (4). If they do not, say that when you grossed the specimen, you only found four lymph nodes. Hopefully, they will tell you the requirements needed for lymph node sampling and that you need to go back and sample more lymph nodes. | Next ask the resident to look at the lymph node. Inform the resident that it is your process to remove the lymph node if it appears prominent during surgery. If the resident correctly identifies metastatic thyroid carcinoma within the node, act surprised. Ask the resident if they are sure and to explain to you why they think it is thyroid carcinoma. Ask the resident if it could be heterotopic thyroid tissue. Inform the resident that you will be sending the thyroid gland shortly. If the resident does not identify the carcinoma, tell them you were concerned because you know the patient had a thyroid mass in the past and you see it now during the procedure. See if the resident rescans the slide to double check their work. If not, tell them you may be sending a hemithyroidectomy and that you would hate to have to go back to operate as this patient is very anxious about any procedure. If they are still confident that the node is negative, ask them to look at the last case. | Next ask the resident if there are some “stains” that could be done to prove if this is “malignant or not.” The resident should explain to you that this diagnosis does not depend on staining but rather on histologic features and the absence of invasion. |
| Tell the “senior resident” you have a silly question: how would I know this is not metastatic breast carcinoma? Hopefully, the “senior resident” will explain that in many cases of colorectal cancer, you can see a precursor dysplastic lesion and that it is unlikely for breast cancer to metastasize to the colon. Ask if there are any immunohistochemical stains that you could use to distinguish breast from colorectal carcinoma. You are looking for the resident to answer CK7, CK20, and other markers such as GATA-3, ER, and PR. Finally, you will want to discuss microsatellite instability testing, BRAF, and Kras testing. The resident will relay a plan for follow-up on the case and explain a practice on how to resample for lymph nodes. If prompted about lymph nodes, you will tell the “senior resident” that your plan is to regross the fat to look for lymph nodes and ask if there are any stains or things that you want done for the case. If they ask about the synoptic worksheet, ask how you fill out the synoptic worksheet and hand it to them. When they get to microsatellite instability and molecular testing, ask them why you need to do this. Finish up by saying you will order blank stains for molecular studies. | The resident will look at the remaining “parathyroid” frozen section. Tell them you saw this and thought it was another parathyroid gland or lymph node. If the resident identifies the tissue as parathyroid, act surprised and say that your error rate for gross prediction of parathyroid vs lymph node is very poor. If they identify the tissue as lymph node and seem confident and satisfied, tell them that you are going to close and discuss a hemithyroidectomy with the patient after she heals from this procedure and repeats another FNA. During this encounter, ask the resident to tell you why they think it is a lymph node. If the resident identifies the tissue as thymus, seem interested and ask the resident to explain to you why they think it is thymus. End the encounter by thanking them and ask them to give you a synopsis of what the diagnoses are, then leave the room. | Finally, mention to the resident that the cyst was a lot larger than what you see on the slides, and ask if they should process more tissue for frozen diagnosis. If the resident asks, say it was at least 10 cm. The resident should be able to discuss how selected areas are chosen for frozen-section diagnosis and the limitations of frozen sections for larger specimens. Finish by thanking the resident and asking for a summary of the findings and their recommendations. |
FNA, fine-needle aspiration; OSPE, Objective Structured Pathology Examination; PTH, parathyroid hormone.
| First Simulation . | Second Simulation . | This Simulation . |
|---|---|---|
| When the resident taking the OSPE enters the room, you, the “junior resident,” are sitting at the microscope waiting for them to begin looking at the slides. You introduce yourself as the “junior resident” and say we have a colon cancer case to look at and hand the slides over with a printed version of the report. If the resident does not ask to look at the gross description or images, ask the resident if they would like to see pictures of the gross. Describe the tumor location in the ascending colon and features (ulcerated mucosa with rolled edges). If the resident does not read the gross description at this time, tell them you were not sure how to describe it and ask if they can check over your gross description. The first two slides are margin slides; explain that you took these as a margin and ask if the lesion was closer, how you might have taken the margins. The next three slides are from the tumor. You let the senior resident look over the slides for 5 minutes or so. Following this time, you tell them that you thought this was a poorly differentiated tumor. Hopefully, they will correct you that this is a well to moderately differentiated tumor, but if not, ask for how you evaluate tumor differentiation. The items you are looking for the resident to discuss are: a. Depth of invasion: this tumor extends to and perforates the peritoneum. Tell the resident the only other colon cancer you grossed was a rectal cancer, and you remember the mesorectum being important. They should be able to discuss the evaluation of the mesorectum completeness. b. Margin status: the tumor is within 1 cm from the radial margin. Ask the resident what the radial margin is, as you read it in the books you were reading. c. Lymphovascular and perineural invasion | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You comment on how fast the pathology assistant grossed and prepared the frozen section. You then start out by saying, “So my parathyroid is 0.4 g, what do you think of that, Dr. X?” in a jovial way. If the resident does not acknowledge that this is enlarged, follow up the statement with, “Do you think that qualifies for adenoma?” Then ask the resident if they can look at the parathyroid first before the prelaryngeal node as you are so curious to see it. Ask the resident if the parathyroid is cellular and if it is consistent with an adenoma. The resident may inquire about intraoperative PTH levels and respond that they decreased following removal of the lesion. | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You mention that you thought this would be an easy case, but the cyst looked a little suspicious. Allow the resident around 5 minutes to evaluate the slides, then ask for the diagnosis. If the resident incorrectly identifies this borderline serous tumor as a more benign lesion, you may lead them toward the correct diagnosis by asking about the patterns you see (“Is this some kind of papillary thing? What’s that purple stuff?”). If they incorrectly call it a serous carcinoma, you may ask them to point out the invasion for you. Once you have gotten to the diagnosis, say, “I’m a little confused. Is this malignant, or not? Do I need to take more out?” The resident should be able to discuss with you the risk of serous borderline tumor, including the risk of recurrence and small possibility of development of serous carcinoma in the future. If the resident brings up the possibility of peritoneal implants or biopsies, you may state that you will consider this back in the operating room. |
| After the resident looks at all the slides, see if they comment on the number of lymph nodes (4). If they do not, say that when you grossed the specimen, you only found four lymph nodes. Hopefully, they will tell you the requirements needed for lymph node sampling and that you need to go back and sample more lymph nodes. | Next ask the resident to look at the lymph node. Inform the resident that it is your process to remove the lymph node if it appears prominent during surgery. If the resident correctly identifies metastatic thyroid carcinoma within the node, act surprised. Ask the resident if they are sure and to explain to you why they think it is thyroid carcinoma. Ask the resident if it could be heterotopic thyroid tissue. Inform the resident that you will be sending the thyroid gland shortly. If the resident does not identify the carcinoma, tell them you were concerned because you know the patient had a thyroid mass in the past and you see it now during the procedure. See if the resident rescans the slide to double check their work. If not, tell them you may be sending a hemithyroidectomy and that you would hate to have to go back to operate as this patient is very anxious about any procedure. If they are still confident that the node is negative, ask them to look at the last case. | Next ask the resident if there are some “stains” that could be done to prove if this is “malignant or not.” The resident should explain to you that this diagnosis does not depend on staining but rather on histologic features and the absence of invasion. |
| Tell the “senior resident” you have a silly question: how would I know this is not metastatic breast carcinoma? Hopefully, the “senior resident” will explain that in many cases of colorectal cancer, you can see a precursor dysplastic lesion and that it is unlikely for breast cancer to metastasize to the colon. Ask if there are any immunohistochemical stains that you could use to distinguish breast from colorectal carcinoma. You are looking for the resident to answer CK7, CK20, and other markers such as GATA-3, ER, and PR. Finally, you will want to discuss microsatellite instability testing, BRAF, and Kras testing. The resident will relay a plan for follow-up on the case and explain a practice on how to resample for lymph nodes. If prompted about lymph nodes, you will tell the “senior resident” that your plan is to regross the fat to look for lymph nodes and ask if there are any stains or things that you want done for the case. If they ask about the synoptic worksheet, ask how you fill out the synoptic worksheet and hand it to them. When they get to microsatellite instability and molecular testing, ask them why you need to do this. Finish up by saying you will order blank stains for molecular studies. | The resident will look at the remaining “parathyroid” frozen section. Tell them you saw this and thought it was another parathyroid gland or lymph node. If the resident identifies the tissue as parathyroid, act surprised and say that your error rate for gross prediction of parathyroid vs lymph node is very poor. If they identify the tissue as lymph node and seem confident and satisfied, tell them that you are going to close and discuss a hemithyroidectomy with the patient after she heals from this procedure and repeats another FNA. During this encounter, ask the resident to tell you why they think it is a lymph node. If the resident identifies the tissue as thymus, seem interested and ask the resident to explain to you why they think it is thymus. End the encounter by thanking them and ask them to give you a synopsis of what the diagnoses are, then leave the room. | Finally, mention to the resident that the cyst was a lot larger than what you see on the slides, and ask if they should process more tissue for frozen diagnosis. If the resident asks, say it was at least 10 cm. The resident should be able to discuss how selected areas are chosen for frozen-section diagnosis and the limitations of frozen sections for larger specimens. Finish by thanking the resident and asking for a summary of the findings and their recommendations. |
| First Simulation . | Second Simulation . | This Simulation . |
|---|---|---|
| When the resident taking the OSPE enters the room, you, the “junior resident,” are sitting at the microscope waiting for them to begin looking at the slides. You introduce yourself as the “junior resident” and say we have a colon cancer case to look at and hand the slides over with a printed version of the report. If the resident does not ask to look at the gross description or images, ask the resident if they would like to see pictures of the gross. Describe the tumor location in the ascending colon and features (ulcerated mucosa with rolled edges). If the resident does not read the gross description at this time, tell them you were not sure how to describe it and ask if they can check over your gross description. The first two slides are margin slides; explain that you took these as a margin and ask if the lesion was closer, how you might have taken the margins. The next three slides are from the tumor. You let the senior resident look over the slides for 5 minutes or so. Following this time, you tell them that you thought this was a poorly differentiated tumor. Hopefully, they will correct you that this is a well to moderately differentiated tumor, but if not, ask for how you evaluate tumor differentiation. The items you are looking for the resident to discuss are: a. Depth of invasion: this tumor extends to and perforates the peritoneum. Tell the resident the only other colon cancer you grossed was a rectal cancer, and you remember the mesorectum being important. They should be able to discuss the evaluation of the mesorectum completeness. b. Margin status: the tumor is within 1 cm from the radial margin. Ask the resident what the radial margin is, as you read it in the books you were reading. c. Lymphovascular and perineural invasion | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You comment on how fast the pathology assistant grossed and prepared the frozen section. You then start out by saying, “So my parathyroid is 0.4 g, what do you think of that, Dr. X?” in a jovial way. If the resident does not acknowledge that this is enlarged, follow up the statement with, “Do you think that qualifies for adenoma?” Then ask the resident if they can look at the parathyroid first before the prelaryngeal node as you are so curious to see it. Ask the resident if the parathyroid is cellular and if it is consistent with an adenoma. The resident may inquire about intraoperative PTH levels and respond that they decreased following removal of the lesion. | When the resident taking the OSPE enters the room, you are sitting at the microscope waiting for the pathologist to begin looking at the slides. You mention that you thought this would be an easy case, but the cyst looked a little suspicious. Allow the resident around 5 minutes to evaluate the slides, then ask for the diagnosis. If the resident incorrectly identifies this borderline serous tumor as a more benign lesion, you may lead them toward the correct diagnosis by asking about the patterns you see (“Is this some kind of papillary thing? What’s that purple stuff?”). If they incorrectly call it a serous carcinoma, you may ask them to point out the invasion for you. Once you have gotten to the diagnosis, say, “I’m a little confused. Is this malignant, or not? Do I need to take more out?” The resident should be able to discuss with you the risk of serous borderline tumor, including the risk of recurrence and small possibility of development of serous carcinoma in the future. If the resident brings up the possibility of peritoneal implants or biopsies, you may state that you will consider this back in the operating room. |
| After the resident looks at all the slides, see if they comment on the number of lymph nodes (4). If they do not, say that when you grossed the specimen, you only found four lymph nodes. Hopefully, they will tell you the requirements needed for lymph node sampling and that you need to go back and sample more lymph nodes. | Next ask the resident to look at the lymph node. Inform the resident that it is your process to remove the lymph node if it appears prominent during surgery. If the resident correctly identifies metastatic thyroid carcinoma within the node, act surprised. Ask the resident if they are sure and to explain to you why they think it is thyroid carcinoma. Ask the resident if it could be heterotopic thyroid tissue. Inform the resident that you will be sending the thyroid gland shortly. If the resident does not identify the carcinoma, tell them you were concerned because you know the patient had a thyroid mass in the past and you see it now during the procedure. See if the resident rescans the slide to double check their work. If not, tell them you may be sending a hemithyroidectomy and that you would hate to have to go back to operate as this patient is very anxious about any procedure. If they are still confident that the node is negative, ask them to look at the last case. | Next ask the resident if there are some “stains” that could be done to prove if this is “malignant or not.” The resident should explain to you that this diagnosis does not depend on staining but rather on histologic features and the absence of invasion. |
| Tell the “senior resident” you have a silly question: how would I know this is not metastatic breast carcinoma? Hopefully, the “senior resident” will explain that in many cases of colorectal cancer, you can see a precursor dysplastic lesion and that it is unlikely for breast cancer to metastasize to the colon. Ask if there are any immunohistochemical stains that you could use to distinguish breast from colorectal carcinoma. You are looking for the resident to answer CK7, CK20, and other markers such as GATA-3, ER, and PR. Finally, you will want to discuss microsatellite instability testing, BRAF, and Kras testing. The resident will relay a plan for follow-up on the case and explain a practice on how to resample for lymph nodes. If prompted about lymph nodes, you will tell the “senior resident” that your plan is to regross the fat to look for lymph nodes and ask if there are any stains or things that you want done for the case. If they ask about the synoptic worksheet, ask how you fill out the synoptic worksheet and hand it to them. When they get to microsatellite instability and molecular testing, ask them why you need to do this. Finish up by saying you will order blank stains for molecular studies. | The resident will look at the remaining “parathyroid” frozen section. Tell them you saw this and thought it was another parathyroid gland or lymph node. If the resident identifies the tissue as parathyroid, act surprised and say that your error rate for gross prediction of parathyroid vs lymph node is very poor. If they identify the tissue as lymph node and seem confident and satisfied, tell them that you are going to close and discuss a hemithyroidectomy with the patient after she heals from this procedure and repeats another FNA. During this encounter, ask the resident to tell you why they think it is a lymph node. If the resident identifies the tissue as thymus, seem interested and ask the resident to explain to you why they think it is thymus. End the encounter by thanking them and ask them to give you a synopsis of what the diagnoses are, then leave the room. | Finally, mention to the resident that the cyst was a lot larger than what you see on the slides, and ask if they should process more tissue for frozen diagnosis. If the resident asks, say it was at least 10 cm. The resident should be able to discuss how selected areas are chosen for frozen-section diagnosis and the limitations of frozen sections for larger specimens. Finish by thanking the resident and asking for a summary of the findings and their recommendations. |
FNA, fine-needle aspiration; OSPE, Objective Structured Pathology Examination; PTH, parathyroid hormone.
The first simulated scenario consisted of a general surgical pathology sign-out with an emphasis on how effectively the resident could describe microscopic findings and communicate their importance in their “report,” specifically related to cancer diagnosis and the information required in a complete report.
The second simulated case consisted of a frozen-section encounter that contained an unexpected malignancy and centered on the communication and interaction with the attending surgeon regarding the pathologic diagnosis and their request for additional information.
The third simulated scenario consisted of a frozen-section encounter that contained an ovarian tumor and centered on communication with an attending surgeon regarding the risks of the lesion and potential limitations of frozen-section diagnosis.
The resident was given the clinical history, instructions, and a general list of tasks prior to entering the room (Table 1). The only room requirements were a microscope with working pointer, a notepad with pen, two chairs, and a telephone.
The second component of the session consisted of four short surgical pathology cases that tested both the resident’s diagnostic skill as well as the ability to identify problems focused on quality assurance. This section was developed with the group of pathologists and a quality specialist. Each of the four cases consisted of a set of microscopic slides, requisition paperwork, gross description, and/or pictures. The residents were not told these cases contained preanalytic issues. Case A was labeled a “mass.” The material on the slide provided did not explain or feasibly correlate with a clinical mass, requiring the resident to recognize the need for further gross examination, review of the patient’s clinical history, and review of prior pathology materials. Case B presented the residents with slides in which the tissue had been poorly processed, with a large hole in the center, requiring the resident to recognize the need to review the gross description and request a recut of the tissue after examining the block. Case C presented the resident with two slides showing squamous carcinoma from a specimen labeled “left leg, possible recurrence” and a gross description that mentioned submitting only one cassette, requiring the resident to recognize the need to discuss the case with the “tech” and request that more tissue be submitted on the case. Case D consisted of a biopsy specimen of an invasive adenocarcinoma of the colon, whereas the clinical information stated the patient was 14 years old, requiring the resident to recognize the need to double check the requisition, bottles, and clinical history for possible specimen mislabeling. The information, including the diagnosis, quality assurance (QA) issue, and possible corrective actions provided to the attending evaluators, is shown in Table 3.
| Cases with preanalytic QA issues: The resident taking part in the OSPE will be asked to evaluate the case and make recommendations for a course of action for the next steps. Below are descriptions of the cases. |
| Case A: Incomplete examination of material to explain a clinical mass |
| Case A: The clinical information states that there is a mass. There is one slide that does not definitively show any mass. Only one section was submitted. |
| Course of action: Obtain radiology and more clinical history, look up any prior surgical materials for review, and ask the grosser to submit the entire specimen. |
| Case B: Poor processing and cutting |
| Case B: The clinical information states there is a breast mass. The slides show the tissue is poorly processed with a large hole in the center. |
| Course of action: Reprocess the tissue, obtain the radiology and clinical history, speak to the person who grossed the tissue, and get a deeper section on the tissue after examining the block. |
| Case C: Discrepancy of gross description and histology slides |
| Case C: The clinical information states “left leg tissue, possible recurrence.” The gross description only describes one section (1A) and no ink. The resident is a given slides 1A and 1B, which show an invasive squamous cell carcinoma. |
| Course of action: Return to the grossing tech to discuss the case. Submit all the tissue and correlate with prior surgical pathology. |
| Case D: Clinical information inconsistent with slide diagnosis |
| Case D: The clinical information states the patient’s age is 14. There is an invasive adenocarcinoma of the colon on the biopsy. |
| Course of action: Double check the requisition, the bottles, and clinical history. |
| Cases with preanalytic QA issues: The resident taking part in the OSPE will be asked to evaluate the case and make recommendations for a course of action for the next steps. Below are descriptions of the cases. |
| Case A: Incomplete examination of material to explain a clinical mass |
| Case A: The clinical information states that there is a mass. There is one slide that does not definitively show any mass. Only one section was submitted. |
| Course of action: Obtain radiology and more clinical history, look up any prior surgical materials for review, and ask the grosser to submit the entire specimen. |
| Case B: Poor processing and cutting |
| Case B: The clinical information states there is a breast mass. The slides show the tissue is poorly processed with a large hole in the center. |
| Course of action: Reprocess the tissue, obtain the radiology and clinical history, speak to the person who grossed the tissue, and get a deeper section on the tissue after examining the block. |
| Case C: Discrepancy of gross description and histology slides |
| Case C: The clinical information states “left leg tissue, possible recurrence.” The gross description only describes one section (1A) and no ink. The resident is a given slides 1A and 1B, which show an invasive squamous cell carcinoma. |
| Course of action: Return to the grossing tech to discuss the case. Submit all the tissue and correlate with prior surgical pathology. |
| Case D: Clinical information inconsistent with slide diagnosis |
| Case D: The clinical information states the patient’s age is 14. There is an invasive adenocarcinoma of the colon on the biopsy. |
| Course of action: Double check the requisition, the bottles, and clinical history. |
OSPE, Objective Structured Pathology Examination; QA, quality assurance.
| Cases with preanalytic QA issues: The resident taking part in the OSPE will be asked to evaluate the case and make recommendations for a course of action for the next steps. Below are descriptions of the cases. |
| Case A: Incomplete examination of material to explain a clinical mass |
| Case A: The clinical information states that there is a mass. There is one slide that does not definitively show any mass. Only one section was submitted. |
| Course of action: Obtain radiology and more clinical history, look up any prior surgical materials for review, and ask the grosser to submit the entire specimen. |
| Case B: Poor processing and cutting |
| Case B: The clinical information states there is a breast mass. The slides show the tissue is poorly processed with a large hole in the center. |
| Course of action: Reprocess the tissue, obtain the radiology and clinical history, speak to the person who grossed the tissue, and get a deeper section on the tissue after examining the block. |
| Case C: Discrepancy of gross description and histology slides |
| Case C: The clinical information states “left leg tissue, possible recurrence.” The gross description only describes one section (1A) and no ink. The resident is a given slides 1A and 1B, which show an invasive squamous cell carcinoma. |
| Course of action: Return to the grossing tech to discuss the case. Submit all the tissue and correlate with prior surgical pathology. |
| Case D: Clinical information inconsistent with slide diagnosis |
| Case D: The clinical information states the patient’s age is 14. There is an invasive adenocarcinoma of the colon on the biopsy. |
| Course of action: Double check the requisition, the bottles, and clinical history. |
| Cases with preanalytic QA issues: The resident taking part in the OSPE will be asked to evaluate the case and make recommendations for a course of action for the next steps. Below are descriptions of the cases. |
| Case A: Incomplete examination of material to explain a clinical mass |
| Case A: The clinical information states that there is a mass. There is one slide that does not definitively show any mass. Only one section was submitted. |
| Course of action: Obtain radiology and more clinical history, look up any prior surgical materials for review, and ask the grosser to submit the entire specimen. |
| Case B: Poor processing and cutting |
| Case B: The clinical information states there is a breast mass. The slides show the tissue is poorly processed with a large hole in the center. |
| Course of action: Reprocess the tissue, obtain the radiology and clinical history, speak to the person who grossed the tissue, and get a deeper section on the tissue after examining the block. |
| Case C: Discrepancy of gross description and histology slides |
| Case C: The clinical information states “left leg tissue, possible recurrence.” The gross description only describes one section (1A) and no ink. The resident is a given slides 1A and 1B, which show an invasive squamous cell carcinoma. |
| Course of action: Return to the grossing tech to discuss the case. Submit all the tissue and correlate with prior surgical pathology. |
| Case D: Clinical information inconsistent with slide diagnosis |
| Case D: The clinical information states the patient’s age is 14. There is an invasive adenocarcinoma of the colon on the biopsy. |
| Course of action: Double check the requisition, the bottles, and clinical history. |
OSPE, Objective Structured Pathology Examination; QA, quality assurance.
Scoring
Each OSPE scenario was scored based on the Pathology Milestones deemed relevant to that specific encounter, using the 0 to 4 scoring guidelines provided by the ACGME. The ACGME Milestones were the basis of the rubric used by the attending evaluator for formative assessment for the simulated interactions. The case and slides were chosen by a task force group of pathologists interested in resident education. Due to time constraints of the available attendings, the attending evaluator also played the standardized role. The attending evaluator spent 1 hour learning how to play a standardized role by reviewing the script. A detailed sample of the scripts for the simulated cases is in Table 2. In the first simulated case, the evaluator was also instructed to answer questions as if they were the person who grossed the specimen. In all, 13 of the milestones were evaluated.
The QA section, consisting of the four case-based sections, were scored based on if the resident was able to correctly describe and identify the preanalytic problem and solution(s) available. This section was scored on a 0 to 2 scale with three components: diagnosis, QA issue, and follow-up action. For each component, a score of 0 was given if nothing was recognized, a score of 1 if there was partial recognition, and a score of 2 if completely identified. The highest total score was 6 for each case and 24 for all four cases.
Following the simulated experience, the residents received immediate verbal feedback on their performance and had an opportunity to discuss the encounter with the evaluator. Later, the resident received the written narrative feedback via the electronic evaluation system and their ACGME Milestone level based on the rubric. The resident received the correct preanalytic issues and written feedback on their performance on the QA section 1 week later, and a debrief session was held to go over the preanalytic issues presented in the cases.
Results
The average milestone score was 1.4 out of 5 for first-year residents and 2.3 out of 5 for second-year residents. Individual residents’ average scores ranged from 1 to 3.5, as shown in Figure 1. This was slightly lower than the historic average milestones for PGY-1 level residents obtained from more traditional means and around the same for PGY-2 level residents. Table 4 contains the individual data for milestone scores, by resident year. There was an overall improvement in the milestone level of the residents who were assessed over both of the years the OSPE was given, as shown in Figure 2.
| . | Milestone . | . | . | . | . | . | . | . | . | . | . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | ICS1 . | ICS2 . | MK1 . | MK2 . | PBLI1 . | PC1 . | PC2 . | PC3 . | PC4 . | PC5 . | PC7 . | PROF4 . | SBP1 . |
| PGY-1 residents | |||||||||||||
| Res A | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1 | 2 | 1 |
| Res B | 1 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res C | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1 | 1 | 2 | 1 |
| Res D | 2 | 2 | 2 | 2.5 | 1.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 |
| Res E | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Res F | 1.5 | 1.5 | 2 | 3 | 2 | 1 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 3 | 2 |
| Res G | 1 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1.5 |
| Res H | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.5 | 1 | 1 | 1.5 | 1 |
| Res I | 1 | 1 | 1.5 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Red J | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res K | 2 | 2.5 | 1 | 2 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res L | 2 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res M | 2 | 1.5 | 2 | 2 | 2 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 |
| Res N | 1.5 | 1 | 1 | 1 | 2 | 1 | 2 | 1.5 | 1 | 1.5 | 1 | 2 | 1 |
| PGY-2 residents | |||||||||||||
| Res A | 2 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2 | 2 | 2.5 | 2 |
| Res B | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Res C | 2 | 2 | 2 | 2.5 | 3 | 2 | 2.5 | 2 | 2.5 | 2 | 2 | 3 | 2 |
| Res D | 3 | 2.5 | 2.5 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 3 | 2.5 |
| Res E | 2 | 2 | 2 | 1.5 | 2 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 1.5 |
| Res F | 3 | 2.5 | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 2.5 | 2 | 3 | 2.5 |
| Res G | 2 | 2 | 2 | 3 | 3 | 2 | 1.5 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res H | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 | 2 | 2.5 | 2 | 2 | 2 |
| Res O | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res P | 1.5 | 1.5 | 2 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res Q | 3.5 | 3 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 4 | 3.5 | 3.5 | 3.5 |
| Res R | 2.5 | 2 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 |
| Res S | 2 | 1.5 | 2 | 2.5 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 | 2 |
| Res T | 2.5 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2.5 |
| Res U | 2 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| . | Milestone . | . | . | . | . | . | . | . | . | . | . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | ICS1 . | ICS2 . | MK1 . | MK2 . | PBLI1 . | PC1 . | PC2 . | PC3 . | PC4 . | PC5 . | PC7 . | PROF4 . | SBP1 . |
| PGY-1 residents | |||||||||||||
| Res A | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1 | 2 | 1 |
| Res B | 1 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res C | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1 | 1 | 2 | 1 |
| Res D | 2 | 2 | 2 | 2.5 | 1.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 |
| Res E | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Res F | 1.5 | 1.5 | 2 | 3 | 2 | 1 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 3 | 2 |
| Res G | 1 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1.5 |
| Res H | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.5 | 1 | 1 | 1.5 | 1 |
| Res I | 1 | 1 | 1.5 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Red J | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res K | 2 | 2.5 | 1 | 2 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res L | 2 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res M | 2 | 1.5 | 2 | 2 | 2 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 |
| Res N | 1.5 | 1 | 1 | 1 | 2 | 1 | 2 | 1.5 | 1 | 1.5 | 1 | 2 | 1 |
| PGY-2 residents | |||||||||||||
| Res A | 2 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2 | 2 | 2.5 | 2 |
| Res B | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Res C | 2 | 2 | 2 | 2.5 | 3 | 2 | 2.5 | 2 | 2.5 | 2 | 2 | 3 | 2 |
| Res D | 3 | 2.5 | 2.5 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 3 | 2.5 |
| Res E | 2 | 2 | 2 | 1.5 | 2 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 1.5 |
| Res F | 3 | 2.5 | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 2.5 | 2 | 3 | 2.5 |
| Res G | 2 | 2 | 2 | 3 | 3 | 2 | 1.5 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res H | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 | 2 | 2.5 | 2 | 2 | 2 |
| Res O | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res P | 1.5 | 1.5 | 2 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res Q | 3.5 | 3 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 4 | 3.5 | 3.5 | 3.5 |
| Res R | 2.5 | 2 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 |
| Res S | 2 | 1.5 | 2 | 2.5 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 | 2 |
| Res T | 2.5 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2.5 |
| Res U | 2 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
OSPE, Objective Structured Pathology Examination; PGY, postgraduate year.
aBolded residents completed the OSPE both years.
| . | Milestone . | . | . | . | . | . | . | . | . | . | . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | ICS1 . | ICS2 . | MK1 . | MK2 . | PBLI1 . | PC1 . | PC2 . | PC3 . | PC4 . | PC5 . | PC7 . | PROF4 . | SBP1 . |
| PGY-1 residents | |||||||||||||
| Res A | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1 | 2 | 1 |
| Res B | 1 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res C | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1 | 1 | 2 | 1 |
| Res D | 2 | 2 | 2 | 2.5 | 1.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 |
| Res E | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Res F | 1.5 | 1.5 | 2 | 3 | 2 | 1 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 3 | 2 |
| Res G | 1 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1.5 |
| Res H | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.5 | 1 | 1 | 1.5 | 1 |
| Res I | 1 | 1 | 1.5 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Red J | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res K | 2 | 2.5 | 1 | 2 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res L | 2 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res M | 2 | 1.5 | 2 | 2 | 2 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 |
| Res N | 1.5 | 1 | 1 | 1 | 2 | 1 | 2 | 1.5 | 1 | 1.5 | 1 | 2 | 1 |
| PGY-2 residents | |||||||||||||
| Res A | 2 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2 | 2 | 2.5 | 2 |
| Res B | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Res C | 2 | 2 | 2 | 2.5 | 3 | 2 | 2.5 | 2 | 2.5 | 2 | 2 | 3 | 2 |
| Res D | 3 | 2.5 | 2.5 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 3 | 2.5 |
| Res E | 2 | 2 | 2 | 1.5 | 2 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 1.5 |
| Res F | 3 | 2.5 | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 2.5 | 2 | 3 | 2.5 |
| Res G | 2 | 2 | 2 | 3 | 3 | 2 | 1.5 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res H | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 | 2 | 2.5 | 2 | 2 | 2 |
| Res O | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res P | 1.5 | 1.5 | 2 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res Q | 3.5 | 3 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 4 | 3.5 | 3.5 | 3.5 |
| Res R | 2.5 | 2 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 |
| Res S | 2 | 1.5 | 2 | 2.5 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 | 2 |
| Res T | 2.5 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2.5 |
| Res U | 2 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| . | Milestone . | . | . | . | . | . | . | . | . | . | . | . | . |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| . | ICS1 . | ICS2 . | MK1 . | MK2 . | PBLI1 . | PC1 . | PC2 . | PC3 . | PC4 . | PC5 . | PC7 . | PROF4 . | SBP1 . |
| PGY-1 residents | |||||||||||||
| Res A | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1 | 2 | 1 |
| Res B | 1 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res C | 1.5 | 1.5 | 1.5 | 1 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1 | 1 | 2 | 1 |
| Res D | 2 | 2 | 2 | 2.5 | 1.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 |
| Res E | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Res F | 1.5 | 1.5 | 2 | 3 | 2 | 1 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 3 | 2 |
| Res G | 1 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 3 | 1.5 |
| Res H | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1.5 | 1 | 1 | 1.5 | 1 |
| Res I | 1 | 1 | 1.5 | 1 | 1.5 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Red J | 1 | 1 | 1 | 1 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res K | 2 | 2.5 | 1 | 2 | 2 | 1.5 | 1 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res L | 2 | 1 | 1.5 | 2 | 2 | 1 | 1 | 1 | 1 | 1 | 1 | 2 | 1 |
| Res M | 2 | 1.5 | 2 | 2 | 2 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 |
| Res N | 1.5 | 1 | 1 | 1 | 2 | 1 | 2 | 1.5 | 1 | 1.5 | 1 | 2 | 1 |
| PGY-2 residents | |||||||||||||
| Res A | 2 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2 | 2 | 2.5 | 2 |
| Res B | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Res C | 2 | 2 | 2 | 2.5 | 3 | 2 | 2.5 | 2 | 2.5 | 2 | 2 | 3 | 2 |
| Res D | 3 | 2.5 | 2.5 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 2.5 | 3 | 3 | 2.5 |
| Res E | 2 | 2 | 2 | 1.5 | 2 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 1.5 |
| Res F | 3 | 2.5 | 2 | 3 | 3 | 2 | 2 | 2 | 2 | 2.5 | 2 | 3 | 2.5 |
| Res G | 2 | 2 | 2 | 3 | 3 | 2 | 1.5 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res H | 2 | 2 | 2 | 2 | 2 | 2 | 2.5 | 2 | 2 | 2.5 | 2 | 2 | 2 |
| Res O | 2 | 1.5 | 1.5 | 2 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 1.5 | 2 | 2 |
| Res P | 1.5 | 1.5 | 2 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
| Res Q | 3.5 | 3 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 3.5 | 4 | 3.5 | 3.5 | 3.5 |
| Res R | 2.5 | 2 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 | 2.5 |
| Res S | 2 | 1.5 | 2 | 2.5 | 2 | 1.5 | 1.5 | 1.5 | 2 | 1.5 | 2 | 2 | 2 |
| Res T | 2.5 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2.5 | 2.5 | 2 | 2.5 | 2.5 | 2.5 |
| Res U | 2 | 2 | 2.5 | 3 | 2.5 | 2 | 2 | 2 | 2 | 2 | 2 | 3 | 2 |
OSPE, Objective Structured Pathology Examination; PGY, postgraduate year.
aBolded residents completed the OSPE both years.
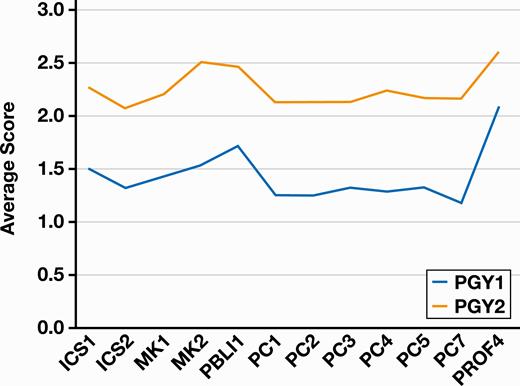
The average milestone score for first postgraduate year (PGY-1) and second postgraduate year (PGY-2) residents.
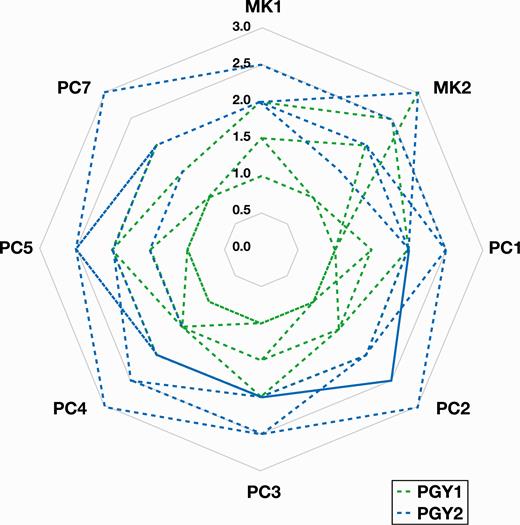
Comparative scores of individual residents accessed during both their first postgraduate (PGY-1) and second postgraduate (PGY-2) years.
For the four surgical pathology cases with QA issues, the average score was 15 of 24 for PGY-1 residents and 11.5 of 24 for PGY-2 residents. Within PGY-1, the average scores for the diagnosis, problem identification, and potential solutions section were 1.5, 1.2, and 1.1, respectively, on the 0 to 2 score scale described above. For PGY-2, the average scores for the diagnosis, problem identification, and potential solutions section were 2, 0.4, and 0.5, respectively.
Discussion
This pathology simulation pilot, OSPE, was a proof-of-concept study demonstrating that the assessment of pathology residents in a simulated environment is possible and may be further developed as a method to assess resident performance, give feedback, and observe overall trends in milestone and other objective fulfillment. The OSPE provides pathology residency programs with a standardized method of evaluation of residents, particularly around topics such as communication skills that do not lend themselves easily to multiple-choice examinations. The OSPE can also identify deficiencies early on in a resident’s training, as well as allowing the program to effectively provide solutions for typical quality and safety issues that occur in the AP laboratory. In our institution, for example, we were able to identify that several of our residents had difficulty identifying the practical preanalytic issues in our QA cases, and even when the error was identified, some could not effectively explain how they would deal with this error. This led us to create additional teaching sessions focused on these issues within our quality and laboratory administration teaching. In addition, the evaluators noted that two residents had difficulty explaining the importance and limitations of frozen section diagnoses to the “surgeons.” Using the OSPE, a program can thus focus resident education by identifying resident weakness and curriculum gaps in training. We posit that further implementation and serial follow-up will improve competency and can be extended even to junior attendings who are new to practice. This is an improvement on the current common practices for pathology education, which involve a generalized curriculum identical for all residents. If time were to be built into the schedule for “competency” rotations, when problem areas are identified for residents, as in our case with quality issues or frozen section communication, this time could be devoted specifically to improvement in these areas. For example, an additional rotation as dealing with frozen sections could be assigned. A long-term goal would be the development of greater flexibility in the pathology resident’s schedule, with OSPE-like assessments helping to determine the rotations needed.
As this method becomes more standard across programs and the pathology milestones better developed, rubrics for readiness related to graduated responsibility can be standardized and globally applied across programs.
With careful planning and vetting, the OSPE has the potential for use in resident assessment in other areas of AP and CP. Rare reports, such as the one written by Olson and George,12 describe the use of simulation in pathology education and training. Focused more on on-call responsibilities, the authors describe a workshop to prepare residents for commonly encountered scenarios. While this workshop did not lay out a method for evaluation of residents, this type of activity could be transformed so that competency was assessed using the OSPE model. Simulation for tumor board presentation or other forms of pathology consultation in AP could be delivered via an OSPE.
The evaluation and assessment of knowledge, skills, and attitudes can be difficult in pathology residency training. In the AP portion of training, many times this evaluation comprises direct observation over the course of a rotation that is linked to a milestone-based electronic evaluation. Some programs give homegrown assessments based on unknown slides or other types of examinations. Other sources of information on resident knowledge for practice are the resident in-service examination and programmatically the board pass rate. While all of these assessments provide crucial information on resident medical knowledge and some information on a resident’s performance, they may miss the opportunity to address a resident’s weakness in translation of these skills to practice. Pathology simulation with feedback provides an objective delineation of behaviors and evaluation of those behaviors for the purposes of informing the residents’ practice pattern. Because of the link to rubrics or scoring, the OSPE can provide metrics for evaluation of resident performance in a variety of specific topics from cancer staging to frozen section evaluation. Over time, pathology programs can follow resident performance and use this to document progression of clinical skills and levels of achievement and areas in need of improvement. The benefits could also extend to attending pathologists in the form of faculty development such as giving feedback.
While simulation-based assessment is not without drawbacks, most issues encountered in this study were logistical. The OSPE required a time commitment by both residents and supervising pathologists. Planning of an OSPE requires specific behavioral anchored metrics to examine and to gather pertinent materials such as slides, gross images, and cases. In addition, the actual simulation requires time where both residents taking the assessment and pathologists administering the assessment are free from clinical duties.
Some of the limitations of this study include the lack of a control group and the use of the attending as an evaluator and standardized role player. As this was a feasibility study, the use of a simulation center with microscope setup and access to trained simulation staff could increase the output of this method and streamline the process. Video capture of the interaction could then also be used for resident instruction. Consistency across evaluators would be evaluated to limit rater bias and ensure alignment with the grading rubric.
Achieving competency in laboratory management, including QA, is an important aspect of any pathology graduate education. The Academy of Directors of Surgical and Anatomic Pathology lists basic QA knowledge on its list of competencies for advancing AP residents.13 In AP, most residents will encounter at least some QA incidents ranging from mislabeled specimens and slides to missing tissue. Most of these events are preanalytic and may be resolved without patient harm (“near misses”) or any sacrifice in quality care when identified promptly. While QA events are tracked for the purposes of departmental quality improvement, recently trained pathologists and employers both cite laboratory management skills, including quality management, as an area of weakness,14 indicating a possible deficiency of training throughout many residency programs. There are few methods to assess a resident’s competence in handling them, as multiple-choice questions fail to discern if a resident would be able to come up with a plan on their own, rather than selecting the best option from a provided list. These aspects make OSCE-style examinations a good option for performance-based assessment of resident physicians specifically related to preanalytic issues in AP. In this study, it was evident that when faced with common preanalytic issues, that resident struggled in identifying the issue and providing potential solutions. This observation informed our curricular change to directly address resident education of preanalytic problems in the AP laboratory.
Conclusion
The use of simulation in this study as a method for standardized assessment provides a starting point for the evaluation of pathology resident milestone competency and QA knowledge. We were able to successfully identify specific areas for improvement for several of our residents and provide corrective action. OSPE examination could play a useful role within pathology postgraduate medical training, especially within the framework of the ACGME’s new accreditation policies. In the current era of accountability set forth by the ACGME, standardized evaluation of these competencies holds great importance for postgraduate pathology training. The use of the OSPE would help ensure that the transition to practice is not solely based on time spent in a residency program and the successful completion of a single standardized examination but rather the ability to successfully navigate situations expected of an attending physician in an open-ended situation, mimicking real-world experience more closely than a multiple-choice examination could.




