-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie R Smith, Martin S Hagger, Jacob J Keech, Susette A Moyers, Kyra Hamilton, Improving Hand Hygiene Behavior Using a Novel Theory-Based Intervention During the COVID-19 Pandemic, Annals of Behavioral Medicine, Volume 56, Issue 11, November 2022, Pages 1157–1173, https://doi.org/10.1093/abm/kaac041
Close - Share Icon Share
Abstract
Promoting the adoption of personal hygiene behaviors known to reduce the transmission of COVID-19, such as avoiding touching one’s face with unwashed hands, is important for limiting the spread of infections.
We aimed to test the efficacy of a theory-based intervention to promote the avoidance of touching one’s face with unwashed hands to reduce the spread of COVID-19.
We tested effects of an intervention employing imagery, persuasive communication, and planning techniques in two pre-registered studies adopting randomized controlled designs in samples of Australian (N = 254; Study 1) and US (N = 245; Study 2) residents. Participants were randomly assigned to theory-based intervention or education-only conditions (Study 1), or to theory-based intervention, education-only, and no-intervention control conditions (Study 2). The intervention was delivered online and participants completed measures of behavior and theory-based social cognition constructs pre-intervention and one-week postintervention.
Mixed-model ANOVAs revealed a significant increase in avoidance of touching the face with unwashed hands from pre-intervention to follow-up irrespective of intervention condition in both studies, but no significant condition effects. Exploratory analyses revealed significant effects of the theory-based intervention on behavior at follow-up in individuals with low pre-intervention risk perceptions in Study 2.
Results indicate high adoption of avoiding touching one’s face with unwashed hands, with behavior increasing over time independent of the intervention. Future research should confirm risk perceptions as a moderator of the effect theory-based interventions on infection-prevention behaviors.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic is a public health emergency of international concern. SARS-CoV-2, the virus that causes COVID-19, is highly contagious, spreading mainly through person-to-person contact. While symptoms of COVID-19 are relatively mild and without serious consequence in most cases [1], modeling data suggest approximately 4% of the global population is at risk of severe COVID-19 if infected [2]. For vulnerable individuals (e.g., the elderly, immunosuppressed individuals, those with underlying health conditions), COVID-19 is a serious and potentially life-threatening disease. Until vaccines have been rolled-out on a global scale, reducing the transmission of COVID-19 and preventing future outbreaks requires the adoption of preventive behaviors known to effectively limit the spread of infections. Promoting wide-scale adoption of personal hygiene practices for preventing the transmission of pathogens is considered particularly important. International guidelines advocate regular hand washing with soap and water and avoiding touching the face, particularly the eyes, nose, and mouth, to avoid infection through transfer of the virus from contaminated surfaces [3]. There is emerging evidence that high rates of adherence to these guidelines is effective in limiting viral transmission [4], with hand hygiene [5, 6] and preventing face touching featuring prominently [7–9].
However, successful behavioral means to prevent infection necessitates widespread compliance. This has prompted researchers in the field of behavior change to call for the identification of potentially efficacious strategies that may promote adoption and maintenance of preventive behaviors, particularly hand hygiene practices, such as avoiding touching the face with unwashed hands, to effectively manage community transmission of the virus [10–12]. However, relatively little is known about the strategies that are efficacious in facilitating adherence to hand hygiene guidelines to minimize spread of the SARS-CoV-2 virus in the context of the current pandemic. Such research may assist in informing public health guidance and developing behavior change interventions likely to promote adherence to hand hygiene behaviors at the population level. The current pre-registered study aimed to address this call by testing the efficacy of an intervention based on behavioral theory to promote increased participation in hand hygiene behavior; specifically, the avoidance of touching one’s face with unwashed hands. The research applied strategies derived from previous theory and evidence that have shown efficacy in promoting behavior change in health contexts by targeting change in key modifiable determinants.
A Theory-Based Intervention Promoting Avoiding Touching the Face with Unwashed Hands
Researchers have advocated the importance of applying behavioral and psychological theory to inform the development of behavior change interventions [13], including researchers during the current pandemic [11, 14]. The promise of such an approach is to identify potentially modifiable psychological determinants of behavior that can be targeted by strategies or techniques included in the content of the intervention. Such an approach also has the advantage of illustrating the mechanisms by which the intervention changes the behavior, and this provides important data on strategies that are most efficacious in particular populations and contexts, and for particular behaviors [15]. The process involves identifying determinants reliably related to the behavior of interest through theory and formative research, and matching evidence-based behavior change strategies or techniques proposed to affect change in the targeted determinants [16–18].
Social cognition approaches have been consistently applied to predict health behavior and inform the development of efficacious behavior change interventions. Prominent among these approaches are the theory of planned behavior (TPB) [19] and health action process approach (HAPA) [20, 21]. These approaches have been shown to be consistently effective in identifying potentially modifiable targets for intervention in many health behavior change contexts, including behaviors aimed at stemming the transmission of the SARS-CoV-2 virus [22–25].
The TPB [19] identifies individuals’ stated intentions to perform the behavior of interest as the most proximal predictor of behavior and mediates effects of three belief-based constructs on behavior performance: attitudes (personal beliefs in the value of performing the behavior), subjective norms (beliefs that significant others support behavioral performance), and perceived behavioral control (beliefs in personal capacity to perform the behavior). The HAPA [20] also specifies intentions as a proximal predictor of behavior, and highlights the importance of outcome expectancies (akin to attitudes from the TPB), risk perceptions (beliefs in the severity of a health condition that may arise from not performing the target behavior and personal vulnerability toward it), and action self-efficacy (akin to perceived behavioral control from the TPB) as determinants of intention and intention as a mediator of their effects of behavior. The HAPA also identifies belief-based factors that facilitate behavioral enactment after intentions have been formed, in a volitional “phase”, which include maintenance self-efficacy (beliefs in being able to maintain behavioral performance), planning (a task-facilitating strategy relating to the preparation of performing a behavior), and action control (individuals’ beliefs about their ability to self-monitor behavioral performance, and to self-regulate effort to ensure behavior is performed to the intended standard).
Social cognition approaches, such as the TPB and the HAPA have been applied extensively to predict health behavior and to inform the development of behavior change interventions [16, 21, 26]. These theories have had demonstrable efficacy in accounting for variance in health behavior [27–29]. Although research applying these theoretical approaches to identify the determinants of COVID-19 preventive behaviors and associated mechanisms is, by comparison, limited, there is emerging evidence that they can be effective in accounting for variance in COVID-19 preventive behaviors [22, 24, 25, 30–34]. For example, prospective correlational evidence indicates the utility of many social cognition constructs that reflect motivational, volitional, and automatic processes in explaining physical distancing behavior in samples of Australian and US community members [23, 24], with longitudinal evidence supporting the sustained effects of these constructs on behavior over time [35].
Taken together, this research provides some initial basis of potentially modifiable constructs that relate to behavior that could be targeted in interventions. Based on these findings, constructs from the TPB and HAPA were used to inform the selection of behavior change strategies used in our intervention aimed at promoting increased avoidance of touching the face with unwashed hands to prevent SARS-CoV-2 transmission. The intervention aimed to develop and test and intervention targeting change in attitude, subjective norm, and perceived behavioral control from the TPB, and risk perception and action planning from the HAPA. These theoretical targets were selected based on prior evidence indicating that they are independent predictors of the target behavior. Strategies or techniques targeting constructs from these theories have also been shown to lead to behavior change in other health behavior contexts [36, 37] and, mediation analyses of intervention research using techniques targeting change in these constructs have demonstrated that intervention effects act by affecting change in these constructs [38, 39]. Specifically, the intervention adopted persuasive communication and mental imagery techniques which targeted behavior change through attitudes, subjective norms, and perceived behavioral control from the TPB, and risk perceptions from the HAPA, and an implementation intention technique which targeted behavior change though the action planning construct from HAPA.
Persuasive communications highlight the advantages of performing a given behavior, and its outcomes have been shown to promote attitude, intention, and behavior change [40]. For example, research reviews and meta-analyses show that such interventions promote simultaneous change in attitudes and behavior in health contexts [40–42]. Mental imagery techniques target change in behavior by promoting positive attitudes and increasing self-efficacy toward performing the behavior in future, and involve individuals mentally representing and rehearsing future actions and consequences [43–45]. Meta-analytic evidence has supported the effectiveness of these imagery techniques on behaviors and social-cognitive constructs [43]. Implementation intentions is a technique in which individuals are promoted to form plans about when, where, and how to enact an intended behavior to achieve a specific goal [46]. Research has supported the effectiveness of implementation intentions in promoting effective enactment of intended behaviors beyond mere formation of a goal intention [47]. The adoption of imagery and implementation intention techniques has been shown to promote behavior change in previous intervention studies [48–52]. Furthermore, implementation intention and mental imagery intervention techniques promote self-initiated behavior change, which can obviate the need for intensive and costly in-person methods [53]. Low-cost and low-burden strategies such as these are desirable in a global pandemic context when a primary objective is to promote widescale adoption of behaviors preventing SARS-CoV-2 transmission without the need for person-to-person contact or expensive practitioner-delivered interventions.
The Present Study
The present pre-registered study aimed to test the efficacy of a brief, theory-based intervention to promote change in avoiding touching the face with unwashed hands. The original intervention design adopted an online two-group randomized controlled design in which the efficacy of an intervention, which comprised persuasive communication, imagery, and implementation intention techniques, in promoting avoiding touching the face with unwashed hands was compared with an education-only message. The intervention was delivered online using resources that can easily be implemented in real-world settings. Both the intervention and education-only condition were also presented with personal hand hygiene guidelines to prevent COVID-19 infection published by World Health Organization [3]. The intervention content was presented following an online survey administered to separate samples of Australian and US residents recruited from online survey panels in each country stratified by age, gender, and area of residence. These two countries experienced rapid increases in COVID-19 cases at relatively similar times during the current pandemic and both introduced public health advice to minimize transmission, including advocating for avoiding touching one’s face with unwashed hands. Participants assigned to the theory-based condition were provided with the WHO guidelines followed by a series of self-enacted exercises in which they were promoted to adopt the theory-based strategies likely to change their behavior: actively make plans to avoid touching their face with unwashed hands; imagining the specific steps required to avoid touching their face with unwashed hands, and mentally rehearsing the feelings if they were to succeed in avoiding touching their face with unwashed hands.
Design Overview and Pre-Registered Hypotheses
The current research comprised two studies. Study 1 tested the efficacy of the theory-based intervention described previously in the cohort from an Australian survey panel. Study 2 was conducted in the cohort from a US survey panel. The lag between recruiting these two cohorts meant that we were able to conduct a pre-registered conceptual replication of the intervention. It afforded us the opportunity to be responsive to findings from Study 1 and modify our design, as necessary. We hypothesized that participants assigned to the theory-based intervention condition would report increased participation in avoiding touching their face with unwashed hands at post-intervention (T2), after adjusting for baseline behavior (T1), relative to those assigned to the control condition. We also predicted increases in measures of the secondary outcome variables (intention, attitude, subjective norm, perceived behavioral control, risk perception, action planning, and action control with respect to the target behavior) at T2 for participants assigned to the theory-based intervention condition relative to participants assigned to the control condition after adjusting each variable for T1 values.
Study 1
Method
Participants
Participants were adult Australian residents (N = 254, 52% men, 47.6% women, 0.04% other) ranging in age from 18 to 82 years (M = 48.37, SD = 17.06). Participants were mostly Caucasian (79.1%), as well as Asian (14.2%), and Middle Eastern (0.8%). The majority of participants had completed tertiary-level education (i.e., Diploma or higher, 73.6%). Participants were eligible for recruitment if they lived in Australia, were aged 18 years or older, and were not currently in formal quarantine for COVID-19, but, at the time of the study, were subject to nationwide “stay at home” orders to prevent the spread of the virus (see Supplementary Material 2, and Supplementary Material 6).
Participants were recruited using a research panel provider (KANTAR Inc.). In addition to the eligibility criteria, participants were screened on the following demographic characteristics and quotas were imposed to ensure that the sample matched the Australian general population on these characteristics: age, gender, and geographic region (by state and metropolitan vs. rural). The COVID-19 restrictions in place in Australia during the period in which the study was conducted were: to stay home unless shopping for essentials, receiving medical care, exercising or travelling to work or education; public gatherings reduced to a maximum of two people (excluding household members); people aged over 70, aged over 60 with pre-existing conditions, or Indigenous people aged over 50 should stay home whenever possible for their own protection.
An a priori statistical power analysis was conducted using G*Power v3.1 for a mixed-model ANOVA estimating fixed effects, main effects, and interactions for the two key independent variables: intervention and time. The effect size was set to detect a small effect (f = 0.18), based on previous research on effectiveness of imagery interventions [43], with power and alpha set at 0.95 and 0.01, respectively, adjusted to protect from inflation of type I error rate due to multiple tests. The analysis returned a minimum required sample size of N = 176 (88 participants in each condition). To allow for 40% attrition, the target sample size was 300 participants at the baseline. As a pre-specified stopping rule, online recruitment ceased once 300 participants had completed the baseline (T1) survey.
Design and procedure
The study was pre-registered prior to data collection on the Open Science Framework: https://osf.io/3rh9u. Griffith University Human Research Ethics Committee approved the study (reference: 2020/199). The study has been reported in accordance with the CONSORT 2010 checklist for reporting randomized trials [54]. Data were collected between April 16 and 28, 2020. Participants completed the online study over two online data collection sessions, one-week apart. In Session 1, participants received study information and provided informed consent, then completed baseline measures of study variables followed by the theory-based intervention or education-only condition materials. In Session 2, participants completed T2 measures of all study variables. See Supplementary Material 1 for full details of the study structure and Supplementary Material 2 for the flow of participants through the study. The study adopted a double-blind parallel two-condition mixed (within-between) randomized controlled design. Participants were not made aware of the condition to which they were assigned and no staff that could have had contact with participants were aware of conditions. Further details of the study design and procedure are available in the study pre-registration document: https://doi.org/10.17605/OSF.IO/3RH9U.
Theory-based intervention development and optimization.
The intervention content was informed by best-practice techniques for mental imagery interventions [43, 52, 55], and based on examples and mechanisms identified in prior research investigating mental imagery intervention techniques in the context of safety behavior promotion [52], stress mindsets [56], and health-related behavior [51, 57]. The intervention was delivered as a slideshow presented on their screen. Participants were required to read a series of slides containing information and instructions for self-enacted hand hygiene exercises and were able to manually advance through the slides. A timer was used on all slides containing intervention stimuli to prevent participants advancing through the information and activities too quickly without fully engaging in the content. Materials for the theory-based intervention and education-only conditions can be accessed online: https://osf.io/uqc6b.
Randomization.
Simple randomization was used to allocate participants to either the theory-based intervention or education-only condition. The randomization was conducted by the Qualtrics randomization feature following completion of the pre-intervention survey. The Qualtrics randomization feature uses a Mersenne Twister pseudorandom number generator which is seeded using a Unix timestamp (in milliseconds).
Education-only condition.
Participants in the education-only condition (i.e., active control condition) were presented only with the educational component of the intervention (i.e., Part 1).
Theory-based intervention condition.
The theory-based intervention condition used a range of behavior change techniques matched with the constructs of the theories adopted in the current study [58]. Behavior change techniques derived from previous theory and evidence that were expected to target change in the identified determinants were selected. Specifically, the intervention adopted persuasive communication, mental imagery, and implementation intention techniques to target change in the TPB and HAPA constructs. Detail of the techniques, the matched targeted theoretical constructs, and implementation strategies employed in the present study are presented in Supplementary Material 3. The content and procedure of the theory-based intervention are outlined in the following sections.
Part 1: Educational Information. Prior to completing the intervention exercises, participants were initially presented with a series of slides containing publicly available educational information on the performance of personal hand hygiene behaviors for preventing the spread of COVID-19 from the World Health Organization website.
Part 2: Formation of a Goal Intention. Participants were then presented with a series of slides adopting persuasive communication to encourage the formation of a goal intention to avoid touching their face with unwashed hands in the next week. Evidence supports the use of persuasive communication to promote attitude, intention, and behavior change [40], with research reviews and meta-analyses showing that such interventions promote simultaneous change in attitudes and behavior in health contexts [40–42]. The way in which the strategy was applied was that participants were guided through a slideshow that included images and messages designed to highlight the potential risks of touching the face with unwashed hands (e.g., contracting the virus themselves; transmitting the virus to others), and to facilitate the visualization of virus transference through hand-to-face contact (e.g., image of a hand touching an escalator handrail contaminated with the virus; an image of a contaminated hand with exaggerated magnification so the virus is visible on the skin). This was developed to target intention, attitudes, and risk perception toward avoiding touching the face with unwashed hands. The slides also included messages describing avoidance of touching the face with unwashed hands as rewarding (i.e., targeting attitude), achievable (i.e., targeting perceived behavioral control), and desirable in the eyes of others (i.e., targeting subjective norm). Following the slides, participants completed a single-item measure of goal intention, indicating their willingness to form a goal to avoid touching their face with unwashed hands in the next week. Participants were presented with the statement “I am willing to form a goal to avoid touching my face with unwashed hands in the next week”, with responses recorded on a 7-point scale (1 = strongly disagree to 7 = strongly agree).
Part 3: Implementation Intention. The next component of the intervention consisted of implementation intentions, a technique in which individuals are prompted to form plans about when, where, and how to enact an intended behavior to achieve a specific goal [46]. This strategy was designed to target change in action planning. Research supports the effectiveness of implementation intentions in promoting effective enactment of intended behaviors beyond mere formation of a goal intention [47]. Participants were first guided through an action planning exercise in which they were instructed to consider when, where, and how they will avoid touching their face with unwashed hands in the next week. Then, to increase the likelihood of following through on their intention, participants recorded their plan using an “if-then” format consistent with suggested guidelines [59, 60]. An example of an “if-then” plan to avoid touching the face with unwashed hands is “If… I visit the supermarket during the next week, then I will… ensure that I avoid touching my face until I have washed my hands afterwards.”
Part 4: Process Imagery or Mental Simulation Exercise. The final components of the intervention comprised mental imagery techniques, in which participants were instructed to mentally represent and rehearse future actions and consequences [43–45]. Imagery is proposed to target change in attitudes and perceived behavioral control or self-efficacy toward the behavior. Meta-analytic evidence and previous intervention studies support the effectiveness of mental imagery techniques on behaviors and social-cognitive constructs [43, 48–52, 61]. Following the previous planning exercise, participants were instructed to imagine situations in which they would avoid touching their face with unwashed hands in the next week and provide a brief summary of the scenarios they imagined in a text entry box. Participants were then instructed to spend a couple of minutes imagining the process involved in avoiding touching their face with unwashed hands in the next week, visualizing themselves carrying out these steps and keeping that picture in their mind. The process imagery exercise was designed to target intention and perceived behavioral control with respect to avoiding touching the face with unwashed hands. Following the imagery exercise, participants recorded a brief summary of their process imagery in a text entry box.
Part 5: Outcome Imagery or Mental Simulation Exercise. Participants were then guided through a second imagery exercise, this time imagining the outcomes of avoiding touching their face with unwashed hands in the next week. Participants were instructed to imagine the benefits of performing the behavior, and the consequences of failing the perform the behavior, which targeted attitudes and risk perception; to picture themselves successfully avoiding touching their face with unwashed hands and imagining the satisfaction that comes with it, which targeted perceived behavioral control; and to imagine how their significant others will feel about their successful performance of the behavior, which targeted subjective norms. Following this, participants typed a brief summary of their outcome imagery into a text entry box.
Treatment fidelity.
Several strategies were implemented to assess and monitor the fidelity of treatment delivery, receipt, and enactment [62]. Please refer to Supplementary Material 4 for a detailed overview of the fidelity assessment and results. The slideshow containing all intervention materials is also available online: https://osf.io/uqc6b.
Measures
Study measures were carried out on multi-item psychometric instruments developed using published guidelines and adapted for use with the target behavior in the current study [20, 63, 64]. All measures were assessed at baseline (T1) and at the one-week (T2) follow-up. All items were rated on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree), unless otherwise specified. See Supplementary Material 5 for items and reliability coefficients for all measures used in the study.
Behavior.
Behavior was defined as “avoiding touching one’s face with unwashed hands,” as recommended by the WHO for preventing pathogen transmission which causes COVID-19. This definition of the behavior is based on survey tool recommendations provided by the WHO for behavioral insight studies related to COVID-19 [65]. The rationale for targeting this behavior is that once contaminated through touching surfaces that potentially harbor the virus in the course of daily living, hands can transfer the virus to individuals’ eyes, nose, or mouth and infect them. Participants were presented with an introductory text: “Hands touch many surfaces and can pick up viruses. Once contaminated, hands can transfer the virus to your eyes, nose, or mouth. From there, the virus can enter your body and can make you sick.” Participants then responded to two questions: (1) “In the past week, how often have you avoided touching your face with unwashed hands?” measured on a 7-point Likert scale (1 = never to 7 = always); (2) “In the past week, I avoided touching my face with unwashed hands” measured on a 7-point Likert scale (1 = false to 7 = true).
Intention.
Three items measured intention to engage in the target behavior in the next week (e.g., “I intend to avoid touching my face with unwashed hands”).
Attitude.
Attitude toward engaging in the target behavior in the next week was measured in response to the common stem: “Avoiding touching my face with unwashed hands in the next week would be….” with responses provided on three 7-point semantic differential scales (1 = unpleasant to 7 = pleasant; 1 = bad to 7 = good; 1 = worthless to 7 = valuable).
Subjective norm.
Four items measured subjective norm with respect to engaging in the target behavior in the next week (e.g., “Other people I know avoid touching their face with unwashed hands”).
Perceived behavioral control.
Four items measured perceived behavioral control with respect to engaging in the target behavior in the next week (e.g., “I have complete control over whether I avoid touching my face with unwashed hands”).
Perceived risk.
Two items measured perceived risk with respect to not engaging in the target behavior in the next week (e.g., “It would be risky for me to not avoid touching my face with unwashed hands”).
Action planning.
Four items measured action planning with respect to engaging in the target behavior in the next week (e.g., “I have made a plan for… when to avoid touching my face with unwashed hands”).
Action control.
Three items measured action control with respect to engaging in the target behavior in the past week (e.g., “I have consistently monitored when, how often, and how to avoid touching my face with unwashed hands”).
Habit.
Habit was defined as the extent to which individuals experienced the behavior as “automatic” and performed “without thinking”. It was measured using Gardner et al.’s [66] four-item version of the original self-reported behavioral automaticity index [67]. These four items focus on the experience of automaticity and omit content relating to behavioral frequency and self-identity (e.g., “Avoiding touching my face with unwashed hands is something I do automatically”).
Anticipated regret.
Three items measured anticipated regret with respect to engaging in the target behavior in the next week (e.g., “If I did not avoid touching my face with unwashed hands in the next week, it would upset me”).
Baseline participant characteristics.
A range of participant characteristics were measured at baseline to examine variability between the groups: gender, age, ethnicity, marital status, parental status, education, employment status, personal income. See Supplementary Material 6 for detailed information about participant baseline characteristics.
Imagery ability.
Individual differences in imagery ability was measured using a 10-item scale drawn from the International Personality Item Pool (IPIP) [68] and designed to measure Factor V (Intellect and Imagination) of Goldberg’s Big-Five Factor Markers [69]. Responses were provided on 5-point scales (1 = very inaccurate to 5 = very accurate). For example, “Typically, I… Have a vivid imagination.”
Data quality.
Two questions were embedded within the T1 survey to assess attentive responding [70]. The questions instruct the choice of a particular answer so that it is not possible to answer the question incorrectly if the item is read carefully (e.g., “Please select option ‘disagree’ to ensure you are paying attention”) [70]. Participants who did not answer both questions correctly at baseline were immediately screened-out of the survey. Goldammer and colleagues Goldammer et al. 70 suggest that checks of this type should be used to guard against inflated item variances, biased item means toward scale midpoints, and increased residual variances of construct indicators, that occur due to careless responding. In addition, a challenge-response “CAPTCHA” was also embedded at the beginning of the online survey to distinguish between genuine human users and automated computer programs.
Data analysis
According to our pre-registered data analysis protocol, we planned to evaluate the effect of the intervention on avoiding touching face with unwashed hands using a 2 (intervention condition: theory-based intervention vs. education-only control) × 2 (time: pre-intervention vs. post-intervention) mixed-model ANOVA. In the analysis, avoiding touching face with unwashed hands was the dependent variable, with condition (theory-based intervention condition vs. education-only condition) the between-participants independent variable and time (baseline, T1 vs. one-week follow-up, T2) the within-participants independent variable. Similarly, the effect of the intervention on the social cognition outcomes was evaluated using a series of 2 × 2 mixed-model ANOVAs. The social cognition constructs (intention, attitude, subjective norm, perceived behavioral control, perceived risk, action planning, and action control) as separate dependent variables with condition as the between-participants independent variable and time as the within-participants independent variable. Additional exploratory analyses for the effect of the intervention on habit and anticipated regret were carried out using a series of 2 × 2 mixed-model ANOVAs with identical design. Individual mixed-model ANOVAs were conducted to test the hypotheses for the secondary outcomes, with a Bonferroni correction applied to control for inflated Type-1 error rate when multiple tests are performed, as we expected the secondary outcomes to be inter-related. Alpha level for inference was also adjusted to 0.01 to protect from inflation of type I error rate due to multiple tests. Where an ANOVA indicated a significant time × condition interaction for any of the outcome variables, simple effects analyses using estimated marginal means were examined for that outcome.
Little’s [71] test indicated that missing data cannot be assumed to have occurred completely at random. Therefore, Expectation-Maximization imputation was not employed, and only complete cases were analyzed. A MANOVA further indicated that there were no statistically significant T1 differences between dropouts (n = 46) and completers (n = 254) on behavior and social cognition factors, F (10, 289) = 1.29, p = .236, ηp2 = 0.043. Baseline demographic characteristics were also compared for dropouts and completers. Participants lost to follow-up were more likely to be women and of younger age. Baseline characteristics of Study 1 participants per condition and attrition status; and results of attrition analyses are available online: https://osf.io/uqc6b.
Results and Discussion
Pre-registered analyses
Aside from the participants who were lost to follow-up, there were no missing data on any of the study variables. Zero-order correlations among Study 1 variables are presented in Supplementary Material 7. Estimated marginal means, standard errors, and 99% confidence intervals of study variables by time and condition are reported in Supplementary Material 8. Data and output files for all analyses are available online: https://osf.io/uqc6b. Estimated marginal means are presented graphically in Fig. 1 for behavior, action control, and perceived behavioral control.
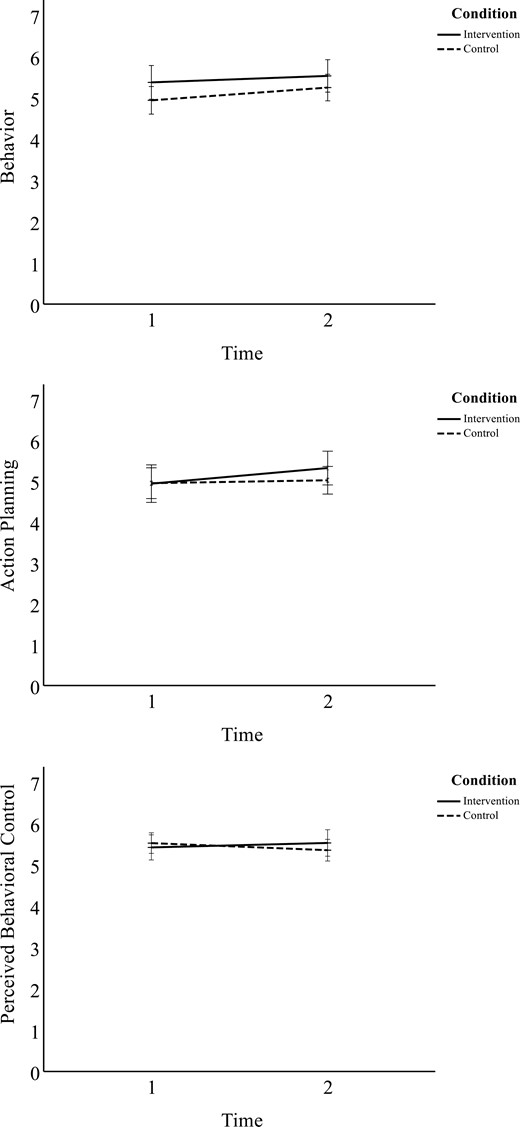
Study 1 behavior, action planning, and perceived behavioral control over time across the intervention and education-only groups. Intervention stimuli delivered between baseline and 1-week follow-up measures. Error bars depict 95% confidence intervals.
Behavior.
We observed a statistically significant main effect of time on avoiding touching the face with unwashed hands, F (1,252) = 8.52, p = .004, ηp2 = .033. Participants reported greater rates of avoiding touching the face with unwashed hands at T2 compared to T1 regardless of condition. However, contrary to predictions, we found no statistically significant time × condition interaction effect, F (1,252) = 0.911, p = .341, ηp2 = 0.004.
Secondary outcomes.
We found a significant main effect of time on action planning, F (1,252) = 8.92, p = .003, ηp2 = 0.034. We also observed a time x condition interaction effect on action planning, F (1,252) = 4.22, p = .041, ηp2 = 0.016; however, it failed to reach statistical significance at the p < .01 level. Follow-up analyses exploring the interaction effect indicated participants assigned to the theory-based intervention condition reported higher levels of action planning at T2 (M = 5.32, SD = 1.61) compared to T1 (M = 4.94, SD = 1.91), F (1,252) = 10.61, p = .001, ηp2 = 0.040. A change in action planning from T1 to T2 was not observed for participants assigned to the education-only condition, F (1,252) = 0.54, p = .463, ηp2 = 0.002.
We also found a time × condition interaction effect on perceived behavioral control, F (1,252) = 5.694, p = .018, ηp2 = .022; however, it failed to reach statistical significance at the p < .01 level. No significant main effects of time or condition were observed. Exploring the interaction effect further, the results of the simple effects analyses also failed to reach statistical significance at the p < .01 level. However, the results indicated that the interaction was explained by an effect of time on the education-only condition, F (1,252) = 5.33, p = .022, ηp2 = 0.02. Participants in the education-only condition reported lower perceived behavioral control at T2 (M = 5.35, SD = 1.29) compared to T1 (M = 5.52, SD = 1.20). There was no effect of time on perceived behavioral control for the theory-based intervention condition. We found no significant main or interaction effects for time and condition on measures of intention, attitude, subjective norm, perceived risk, action control, habit, or anticipated regret.
Overall, our findings revealed statistically significant increases in self-reported avoidance of touching the face with unwashed hands in both intervention and control conditions over time, but no intervention effect. One possible reason for this was that the education component common to both conditions may have been responsible for the observed changes in behavior rather than the imagery intervention. We therefore adjusted the design of our proposed replication in Study 2 by including a further no-education control condition alongside the theory-based intervention and education-only conditions and updated our pre-registration accordingly. We hypothesized that participants allocated to the theory-based intervention and education-only conditions would report higher levels of avoiding face touching with unwashed hands at 1-week follow-up post-intervention (T2) relative to those allocated to the no-education control condition after adjusting for baseline (T1) behavior. We also predicted effects of the theory-based intervention and education-only conditions on secondary outcomes at T2 relative to the no-education control condition after controlling for T1. However, based on the findings of Study 1, we expected no differences between the theory-based intervention and education-only conditions for these outcomes at T2.
Study 2
Method
Participants
Participants were adult US residents (N = 245, 56.7% men) ranging in age from 18 to 84 years (M = 49.51, SD = 16.41). Participants were mostly Caucasian (84.5%), as well as Asian (6.5%), Black (6.1%) and Middle Eastern (.4%). The majority of participants had completed tertiary-level education (i.e., Diploma or higher, 71.5%). Participants were screened against eligibility criteria before entering the trial (see Supplementary Material 2 and Supplementary Material 9). Participants were eligible if they lived in the United States, were aged 18 years or older, and were not currently in formal quarantine for COVID-19. Study 2 followed the same recruitment procedure as Study 1, with age, gender, and location quotas imposed to ensure the sample comprised similar proportions of these characteristics to the general US population. Data were collected between May 19 and June 2, 2020. While there were no nationally mandated COVID-19 restrictions in place in the United States for the period during which the study was conducted, there were state-specific “shelter in place” orders that restricted movement other than for essential tasks (e.g., grocery shopping) or travelling to work for workers in frontline services (e.g., transport, emergency services, healthcare). Some states had begun to ease some of the “shelter in place” orders, but advice on physical distancing and personal hygiene behaviors, including hand sanitizing and avoiding face touching without washing hands, remained in place and promoted by state-wide health advice [72].
A statistical power analysis with the same design and analytic tool as Study 1 was conducted. Results of Study 1 provided the a priori effect size (f = 0.185) and the expected correlations between repeated measures, with power and alpha set a 0.95 and 0.01, respectively. The required sample size was N = 189 (63 participants in each condition). To allow for 40% attrition, the target sample size was 300 participants at T1. Online recruitment ceased once 300 participants completed the T1 survey.
Design and procedure
As before, the study was pre-registered prior to data collection (https://doi.org/10.17605/OSF.IO/RPK3A) and the protocol approved by the University Human Research Ethics Committee (reference: 2020/199). The study has been reported in accordance with the CONSORT 2010 checklist for reporting randomized trials [54]. The study followed the same design as Study 1, with the addition of a third no-education control condition. Participants allocated to the control condition only completed the study measures at T1 and T2. See Supplementary Material 10 for full details of the study structure and Supplementary Material 11 for the flow of participants through the study.
Measures
The same measures of social cognition constructs and behavior from Study 1 were used in Study 2.
Data analysis
In the pre-registered analysis, the effect of the intervention on avoiding touching the face with unwashed hands was evaluated using a 3 (intervention condition: theory-based intervention vs. education-only vs. no-education control) × 2 (time: pre-intervention vs. post-intervention) mixed-model ANOVA. Touching the face with unwashed hands was the dependent variable with condition (theory-based intervention vs. education-only vs. no-education control condition) the between-participants independent variable and time (baseline, T1 vs. one-week follow-up, T2) the within-participants independent variable. Similarly, the effect of the intervention on the social cognition outcomes was evaluated using a series of 3 × 2 mixed-model ANOVAs. The social cognition constructs (intention, attitude, subjective norm, perceived behavioral control, perceived risk, action planning, and action control) as separate dependent variables with condition as the between-participants independent variable and time as the within-participants independent variable. In addition to the pre-registered secondary outcomes outlined, effects of the intervention on habit and anticipated regret were analyzed using a series of 3 × 2 mixed-model ANOVAs with identical design. Alpha level for inference was adjusted to α = 0.01 to protect from inflation of type I error rate due to multiple tests. Where an ANOVA indicated a significant time × condition interaction for any of the outcome variables, simple effects analyses using estimated marginal means were examined for that outcome.
A MANOVA indicated baseline differences between dropouts (n = 74) and completers (n = 245) on behavior and social cognition factors, F (10, 308) = 2.30, p = .013, ηp2 = 0.070. Follow-up analyses indicated higher baseline perceived behavioral control (p = 0.036), intention (p = 0.037), and action planning (p = 0.006) for dropouts compared to completers. Baseline demographic characteristics were compared for dropouts and completers. Participants lost to follow-up were more likely to be women, be of younger age, and have a lower income; and were less likely to be divorced or widowed, to have children, or to have a tertiary level education. Baseline characteristics of Study 2 participants per condition and attrition status, and results of attrition analyses are available online: https://osf.io/uqc6b. As COVID-19 infection rates varied across US states at the time the current study was conducted, we performed an ancillary analysis of the intervention effects on behavior while controlling for rate of COVID-19 infections in US states. Full details and output for the ancillary analyses are available online: https://osf.io/uqc6b.
Results and Discussion
Pre-registered analyses
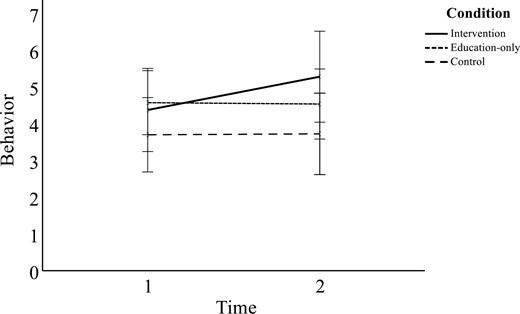
Aside from the participants who were lost to follow-up, there were no missing data on any of the study variables. Zero-order correlations among Study 1 variables are presented in Supplementary Material 12 Estimated marginal means, standard errors, and 99% confidence intervals of study variables by time and condition are reported in Supplementary Material 13 and estimated marginal means for intervention effects are presented graphically in Fig. 2 for behavior, action planning, action control, and habit. Data and output files for all analyses are available online: https://osf.io/uqc6b.

Study 2 behavior, action planning, action control, and habit over time across intervention, education-only, and control groups. Intervention stimuli delivered between baseline and 1-week follow-up measures. Error bars depict 95% confidence intervals.
Behavior.
Consistent with Study 1, we found a statistically significant main effect of time on avoiding touching the face with unwashed hands, F (1,242) = 23.67, p < .001, ηp2 = 0.089, such that uniform increases in avoiding touching the face with unwashed hands were observed from T1 to T2 for all three conditions. We found no statistically significant main effect of condition, F (2,242) = 2.58, p = .078, ηp2 = 0.021, or time × condition interaction effect, F (2,242) = 1.12, p = .328, ηp2 = 0.009, on avoiding touching the face with unwashed hands.
Secondary outcomes.
Several effects were observed for the secondary outcomes: action planning, action control, and habit. However, it must be noted that these effects failed to reach statistical significance at the p < .01 level. We found a main effect of time on action planning, F (1,242) = 4.39, p = .037, ηp2 = 0.018, which was qualified by a time × condition interaction effect, F (2,242) = 4.16, p = .017, ηp2 = 0.033. Simple effects analyses indicated an effect of time on action planning for the theory-based intervention condition, F (1,242) = 5.42, p = .021, ηp2 = 0.022, and the education-only condition, F (1,242) = 4.88, p = .028, ηp2 = 0.020. Participants reported higher levels of action planning at T2 compared to T1 for both these conditions. However, there were no main effects of time or condition on action planning for the control condition.
We also found a main effect of time on action control, F (1,242) = 4.61, p = .033, ηp2 = 0.019, such that all three conditions showed uniform increases in action control from T1 to T2. However, we found no main effect of condition or significant time × condition interaction effect on action control.
While we found no statistically significant main effects of time or condition on habit, we did find a time × condition interaction effect, F (2,242) = 3.20, p = .042, ηp2 = 0.026. Simple effects analyses indicated an effect of time on habit for participants allocated to the theory-based intervention condition, F (1,242) = 4.14, p = .043, ηp2 = 0.017. These participants reported higher levels of habit at T2 compared to T1. There was no main effect of time on habit for the education-only or control conditions. Simple effects analyses indicated an effect of condition on habit at T2, F (2,242) = 5.25, p = .006, ηp2 = 0.042. Pairwise comparisons indicated that participants allocated to the theory-based intervention condition (M = 4.62, SD = 1.28) reported higher levels of habit compared to those allocated to the education-only condition (M = 3.87, SD = 1.28) at T2 (p = .001, d = .59). No main or time or condition interaction effects were observed on habit.
We observed no significant main or interaction effects for time and condition on measures of intention, attitude, subjective norm, perceived behavioral control, perceived risk, or anticipated regret.
Additional exploratory analysis
After conducting the pre-registered analyses and observing non-significant effects of the intervention on behavior in both studies within the overall samples, we used recent empirical research to guide further exploratory analysis. Wise and colleagues [73] reported perceived risk of COVID-19 infection as a significant predictor of protective health behaviors such as physical distancing and hand washing in a US sample. However, they also identified a subset of the US population with low perceived risk of contracting COVID-19 and low engagement in protective behaviors. This subset was identified as potential targets for interventions promoting protective behaviors during the pandemic. Specifically, they predicted people with low perceived risk and low behavioral engagement would most likely benefit most from interventions which target accurate risk development, and also apprise the beneficial effects of their protective behaviors for others, as risk to others may not have been considered to the same extent as personal risk within this subset [73]. Given the current intervention adopted persuasive communications targeting change in risk perceptions and promoting awareness on how an individual is likely to affect others, we identified an opportunity to test Wise and colleagues’ [73] recommendations. Specifically, we tested exploratory hypotheses examining whether participants with lower T1 perceived risk experienced greater benefits from the theory-based intervention than those with higher T1 perceived risk. We hypothesized that there would be a significant effect of the theory-based intervention on behavior for those with lower perceived risk. However, it is important to reiterate that given the exploratory nature of the additional analyses, the results should be interpreted cautiously.
Exploratory analysis procedure
Each sample was divided into two groups based on participant mean T1 score on risk perception. Those with a score less than 5 formed the “low perceived risk” group and those with perceived risk scores greater than or equal to 5 formed the “high perceived risk” group. The rationale for the cut-off was based on the 7-point scale used to assess the two risk perception items, where mean scores <5 represented lower levels of perceived risk (i.e., neutral or lower), and mean scores ≥ 5 represented the presence of perceived risk. A series of 2 (time: T1 vs. T2) × 3 (condition: intervention vs. education-only vs. no-education) × 2 (risk perception: high vs. low) mixed-model ANOVAs on avoiding touching the face with unwashed hands were conducted in both samples to test our exploratory hypotheses. A Bonferroni correction was also applied to control for inflation of Type 1 error rates with multiple tests. Significant three-way interaction effects were investigated further by separate 2 (time: T1 vs. T2) × 3 (condition: intervention vs. education-only vs. no-education) mixed-model ANOVAs for the low and high risk perception groups. For exploratory analyses, α = 0.05 was used as the threshold for statistical significance.
Exploratory analysis results.
We found no significant three-way interaction effect in the Australia sample (Study 1). However, we found a significant three-way interaction effect, F (2,239) = 4.40, p = .013, ηp2 = 0.036, in the US sample (Study 2). To probe the interaction effect, we conducted separate time x condition ANOVAs for those with lower vs. higher perceived risk at T1. Results revealed a significant time x condition interaction effect, F (2,60) = 4.63, p = .013, ηp2 = 0.135, in the low risk perceptions group. Simple effects analyses revealed a significant effect of time on behavior for participants in the theory-based intervention condition, F (1,60) = 12.07, p < .001, ηp2 = 0.168, such that behavior significantly increased from T1 (M = 4.37, SD = 1.43) to T2 (M = 5.28, SD = 1.11; d = 0.71), but not the education-only or control conditions. For participants in the high risk perceptions group, results indicated a main effect of time suggesting uniform increases over time for the three conditions, F (2,179) = 1.62, p < .001, ηp2 = 0.105, and no interaction effects.
Estimated marginal means are presented in Fig. 3 for the effect of the intervention on behavior for the low and high risk perception groups in the US sample. Overall, results of the exploratory analyses suggest that the intervention was successful in promoting avoidance of face touching with unwashed hands in US participants reporting lower risk perceptions at T1. It is important to note, however, that these exploratory analyses did not exceed the statistical significance level commensurate with the criterion we used in the analyses to test our pre-registered intervention effects. As analyses that were not pre-registered, they were not designed to detect effect sizes of this size and at the p < .01 level. Nevertheless, the effects identified in the exploratory analyses are suggestive of the presence of this interaction effect, but warrant further corroboration in a pre-registered study powered to test the specific interaction.
Behavior for US participants with low baseline perceived risk across intervention, education-only, and control groups. Intervention stimuli delivered between baseline and 1-week follow-up measures. Error bars depict 95% confidence intervals.
General Discussion
This preregistered intervention tested the efficacy of a novel theory-based behavior change intervention in promoting the avoidance of face touching with unwashed hands to prevent contracting and spreading COVID-19 in two studies conducted in samples of Australian and US residents, respectively. The intervention adopted persuasive communication, imagery, and implementation intention techniques and aimed to change behavior compared to an education only group that received information on prevention of COVID-19 issued by the WHO [3]. In Study 1, we tested our preregistered hypotheses in the Australian participants. Contrary to our hypotheses, we found no effects of the intervention on behavior in the Australia sample, only uniform increases in self-reported avoidance of touching the face with unwashed hands over time for participants allocated to both conditions. We replicated the intervention in Study 2 in the US sample, and modified our design to include a no-education control group. Results revealed no interaction effects and a similar uniform increase in behavior for participants allocated to all conditions. The intervention did, however, exhibit effects on action planning in both studies, and habit only in Study 2. However, while estimated marginal means of the outcomes were trending favorably in the expected directions for those in the theory-based intervention group at follow-up, effect sizes were small and did not reach statistical significance.
Based on the lack of intervention effects, we conducted additional exploratory analyses of potential moderators of intervention effects. A candidate moderator based on prior research was level of perceived risk of contracting COVID-19. This is based on observed links between risk perceptions and COVID-19 personal protective behaviors [74]. Results indicated significant effects of the intervention on behavior among participants that reported lower T1 risk perceptions, but only among participants in Study 2 (US residents).
Imagery and Planning Intervention Effects
Contrary to our predictions and previous research using imagery and planning interventions to change health behavior [52, 56, 61], we found no effects of the intervention on behavior, and the majority of the secondary outcomes returned null findings. There are several potential explanations for these null findings. The current pattern of findings may reflect two prominent biases in intervention research: the Hawthorne and the “mere-measurement” effects. Hawthorne effects represent effects of participants’ knowledge that they are involved in a study on COVID-19 behaviors, and that they are being “monitored”, on intervention outcomes, while mere measurement effects represent effects of participants’ completion of measures relating to the target behavior on intervention outcomes. Both components have been shown to lead to nontrivial, albeit small effects on behavior [75–77]. So, knowledge of being evaluated may lead participants to alter their responses, particularly their behavior. Similarly, baseline measures of key constructs may, in themselves, serve as an intervention in itself, raising awareness of key attributes or beliefs regarding the target behavior, and leading individuals to change their reports of their beliefs or behavior subsequently. These biases in themselves may not be responsible for the lack of effects of the intervention, but they may have confounded or interfered with the intervention effects. Mere-measurement effects could be isolated in future studies by introducing a no-measurement control group, which would serve as an additional control group to verify the extent of the mere-measurement effect in the current sample. It is more difficult to control for Hawthorne effects, and research suggests that these effects may be ubiquitous across research studies. Nevertheless, given such effects are expected, interventions are expected to have sufficiently robust effects on outcomes regardless of any Hawthorne effects, which does not appear to be the case with the current intervention.
It should be noted that public health campaigns promoting the performance of COVID-19 preventive behaviors such as physical distancing and hand hygiene were highly visible in Australia and the US at the time of data collection for both studies. In addition, international campaigns that were circulating on social media at the time included the United Nations’ Don’t Touch Your Face [78], and the World Health Organization’s Faces Should Be Seen, Not Touched [79] campaigns. The elevated likelihood of exposure to messaging about the risks of contracting the virus and effective measures for avoiding infection raises another possible explanation for the uniform increases to avoidance of touching the face with unwashed hands across all conditions, including the no-education control group in Study 2. Such prominent messaging relating to the target behavior may have had the effect of activating the relevant beliefs (e.g., attitudes, risk perceptions, intentions, planning, and self-monitoring) relevant to the behavior across all conditions. Therefore, one interpretation of the present findings may be that the current intervention did not yield any benefits due to participants prior or current exposure to similar messages.
It is also important to note that participants’ scores on behavior, intention, attitude, subjective norm, perceived behavioral control, and perceived risk were higher than expected in both samples at baseline. Our a priori assumption was that the target behavior was a relatively challenging one to adopt consistently, particularly among those with little experience with this behavior. However, baseline levels appeared to show, in general, good compliance with the behavior (M = 5.11, SD = 1.60 for the Australia sample; M = 5.28, SD = 1.52 for the US sample, each on a 7-point scale), as well as high levels of beliefs in both samples (M range = 4.17–5.88). This suggests that by the time we had implemented the current intervention, many of the participants had already adopted the behavior, possibly in response to public health campaigns in promoting participation in personal protective behaviors, including the target behavior of avoiding touching the face with unwashed hands. This suggests there was relatively limited room for improvement for the behavioral outcome and for many of the social cognition constructs targeted in the intervention.
Another consideration that may have limited intervention efficacy may have been the mode of delivery of intervention components. The intervention exercises were presented as a slideshow, whereas previous studies have used audio and video to guide participants through the exercises [52, 56, 61]. It is possible that individuals felt the attentional effort required to read intervention materials which may have led participants to skip or fail to assimilate the message. However, fidelity measures of the imagery component indicated higher levels of vividness, clarity, detail, and ease with which imagery was performed by intervention participants. Furthermore, previous interventions using text-based intervention delivery have been efficacious in changing behavior [48, 50].
Also noteworthy is the fact that the theory-based intervention in the US sample led to changes in habit, that is, the extent to which avoiding face touching behavior with unwashed hands was experienced as “automatic” and “unthinking”. While the theory-based intervention did not account for the increase in actual behavioral engagement in the present study, the effect on habit suggests its efficacy in increasing the experienced automaticity toward the target behavior. It may have been that the intervention was effective in promoting greater overall context stability of avoiding face touching with unwashed hands, that is, the consistency with which individuals performed the behavior increased even though frequency did not vary [67, 80, 81]. This finding was not observed in the Australia sample. One possible explanation may be that nationwide lockdown orders were implemented earlier in Australia and more uniformly from state to state than in the United States, giving the Australian participants greater opportunity to build habits, that is both frequency and context stability, so the intervention had little effect on either component of habit. However, these interpretations are speculative given that we did not measure the context stability of the target behavior, so we could not unequivocally test whether this was the mechanism behind the effects on habit in the current study. It is also worth noting that the theory-based intervention effect on this construct did not reach the stated level of statistical significance, p < .01.
Another consideration for the present findings may be the use of an intervention strategy that involved planning to avoid doing a behavior in the present research. Research has suggested that planning strategies, such as implementation intentions, may be ineffective for reducing unwanted habits, and may even increase performance of the undesired behavior, when the plan is formed around avoidance of the behavior [82]. A proposed alternative to planning to avoid acting on an impulse is to instead prompt individuals to form an implementation intention to actively ignore the impulse that cues up the behavior when it appears (e.g., “If I have unwashed hands and I feel the urge to touch my face, then I will ignore that urge”). Implementation intentions that specify the ignoring of responses have been found applicable to internal cues such as cravings, and disruptive thoughts and feelings [83], and represents a potentially useful direction for future research testing this strategy to reduce impulsive behavior such as face touching, for limiting virus transmission.
Risk Perceptions as a Moderator
An important finding in the current intervention is the moderation of the intervention effects by risk perceptions in the US sample (Study 2). Given that the current intervention targeted change in risk perceptions, finding that the intervention was effective in participants reporting lower risk perceptions is consistent with Wise and colleagues’ [72] proposition that informing individuals of the beneficial effects of COVID-19 personal protective behaviors for others may increase participation. These findings highlight the imperative of identifying and engaging those with lower perceived risk and developing messages that highlight risks of virus transmission that are effective in this group.
However, that risk perceptions did not moderate intervention effects in the Australia sample suggests some cross-national inconsistency in effects that warrants explanation. To speculate, one possibility is that risk perceptions may not be a relevant determinant or predictor of the target behavior in this sample. For example, a recent prospective correlational study indicated that risk perceptions were a significant predictor of physical distancing intentions and behavior in US participants but not Australian participants [23]. Such evidence suggests that behavior change strategies tapping into risk perceptions may be more effective in groups in which perceived risk or threat is relevant to their formation of intentions to engage in COVID-19 preventive behaviors. In the current context, it may be that Australian participants’ decisions to participate in preventive behaviors was not directly informed by risk perceptions, and perhaps general levels of risk perceptions may have been lower among these participants, when compared to those in the United States for whom risk perceptions are more relevant.
Australia was quicker to contain the spread of the virus and witnessed significantly fewer cases and deaths compared to the United States and the rest of the world, which may have mitigated the size and relevance of risk perceptions in this national group. Furthermore, the timing of data collection for the two studies and the shifting advice on mask-wearing for limiting transmissions may also account for the relevance of risk perceptions potentially differing across the two studies. The Centers for Disease Control and Prevention [84] had initially discouraged mask-wearing, before revising this recommendation in April 2020 and endorsing mask-wearing outside the home to supplement other public health measures such as physical distancing and hand hygiene. Recommendations changed as more evidence emerged about how COVID-19 is spread, and the effectiveness of masks for limiting transmissions [85]. However, while US participants would have been encouraged to wear masks in public at the time of data collection (Study 2, May–June 2020), the first public health recommendation for people to wear masks in public in the state of Victoria in Australia did not occur until July 2020—after Study 1 data collection had finished. Therefore, in addition to the higher case numbers and deaths in the United States, perceived risk may have been more salient for the US sample compared to the Australia sample due to the relatively recent introduction of mask-wearing.
Strengths, Limitations, and Avenues for Future Research
The present research has a number of strengths, particularly its timely focus on a key preventive health behavior aimed at reducing transmission of SARS-CoV-2 to prevent COVID-19 infections, which has not previously been the target of an intervention. Furthermore, the study tested a novel theory-based intervention adopting persuasive communication, imagery, and implementation intentions based on prior research and best practice [43, 52, 56]. The study also used a preregistered randomized controlled design conducted in separate samples of Australian and US residents, stratified by key demographic characteristics.
Current findings, however, should be considered in light of some limitations. First, all outcome measures relied exclusively on self-report and retrospective recall. While the self-report measures used in the intervention exhibited adequate validity and reliability here and in previous research, their use may introduce additional error variance through recall bias and socially desirable responding. Of course, there are challenges to developing nonself-report measures of behaviors such as face touching with unwashed hands, but future studies should consider means by which researchers may gain concurrent validity for the self-report measures, perhaps through covert observation in discreet settings, or by measuring, and then controlling for, social desirability in the model.
Furthermore, the study did not have sufficient statistical power for the additional subgroup analyses conducted examining risk perceptions as a moderator. An important direction for future research would be to replicate these findings with pre-registered hypotheses focusing on the predicted moderator effects of risk perception on intervention effects on face touching behavior with appropriate statistical power. In addition, while there is evidence that relatively simple behaviors can be adopted quickly and that habits can form in a relatively short period of time [86], the 1-week follow-up period precludes any inference of long-term changes to behavior or beliefs in relation to avoiding touching the face with unwashed hands, and we look to future research to investigate the long-term effects of these kinds of interventions on this behavior. Furthermore, meta-analytic evidence indicates that imagery interventions are more effective when the intervention contained a follow-up imagery component (e.g., “booster” text messages, maintaining an imagery-related diary) [43]. Future research may therefore benefit from exploring whether dose moderates intervention effects by delivering an additional follow-up to the imagery component of the intervention.
It must be noted that 15.3% of participants in the Australia sample and 23.3% of participants in the US sample were lost to attrition. Missing data could not be assumed to be missing completely at random and, therefore, complete case analysis was conducted. It is also worth noting that groups disproportionately impacted by additional burdens during the pandemic (i.e., women and those of younger age) [87–89], were more likely to be lost to follow-up in both samples. We also observed high baseline levels of the behavior and associated beliefs in both samples, suggesting relatively little room for improvement. It is probable that the unprecedented nature of the pandemic and the high level of COVID-19 media coverage during the study period could account for the high baseline engagement in this personal protective behavior, as well as the uniform increase in behavioral engagement over time for all conditions. Given the major effects in the current study was time, regardless of the content of the intervention, including a no-education control condition, it seems that mere knowledge of being involved in the study and receiving study measures was sufficient to change participants’ behavior. Replicating the study during a regular flu season during which media exposure will be at a bare minimum and individuals’ vigilance to the illness threat is likely to be low by comparison, may provide a means to control for possible effects of heightened awareness and knowledge and provide a test of intervention effects in the absence of these potential extraneous confounding variables.
We also acknowledge that other preventive behaviors, such as mask wearing and physical distancing, have been identified as particularly salient for COVID-19 prevention. Nevertheless, the promotion of avoiding face touching and hand hygiene behaviors is consistent with research demonstrating the importance of these behaviors in the spread COVID-19 infection [90], justifying our selection. However, it would be prudent to implement interventions that promote uptake of the behaviors targeted here as part of a broader, comprehensive COVID-19 prevention strategy that targets multiple behaviors. Such a strategy may also have the concomitant effect of minimizing transmission of other upper-respiratory viral infections (e.g., the common cold, influenza). We are, however, loath to make definitive recommendations for using the current strategies in interventions aimed at promoting of uptake of other preventive behaviors, or in the prevention of other infections based solely on the current data. Behavior- and illness-specific research is warranted to provide the appropriate evidence base to advocate for the application of the current approach elsewhere.
Finally, individual difference factors such as political affiliation or conspiratorial thinking were not measured in the present research. For example, factors such as a strong endorsement of conservative political beliefs, or beliefs in COVID-19-related conspiracy narratives, are reported to be negatively associated with infection-preventive behavior, vaccination willingness, and perceived risk of COVID-19 to self and others [91, 70]. Exploring avoidance of touching the face with unwashed hands in the context of such individual difference factors may be useful for identifying noncompliant subgroups of the population and tailoring public health messaging accordingly. Furthermore, future studies may wish to explore whether factors such as conspiratorial thinking moderate the effects of an intervention promoting COVID-19 protective behavior.
Conclusion
The current study provided the first test of a theory-based intervention for promoting the COVID-19 personal protective behavior of avoiding touching one’s face with unwashed hands in samples from two different countries, Australia and the United States. In the context of the global pandemic and given the urgent need for populations to adopt COVID-19 personal preventive behaviors, health professionals and behavioral scientists must work together to inform government policy on how to slow the spread of the virus. Until mass inoculation against COVID-19 is achieved, global efforts should continue to focus on reducing the spread of the virus through adoption of behavioral strategies such as proper personal hygiene practices. Even after sufficient widespread immunity to SARS-CoV-2 is achieved, engagement in personal hygiene practices such as avoiding touching the face with unwashed hands will remain relevant for limiting the spread of other viruses such as the flu or common cold.
Overall, present findings indicate high adoption of avoiding touching the face with unwashed hands for limiting the spread of coronavirus among Australian and US residents, with behavioral engagement increasing over time despite the intervention. This may be indicative of the success of public health campaigns targeting hand hygiene behaviors to limit coronavirus transmission. Despite mostly null findings with respect to the hypothesized effects of the intervention, our exploratory analyses provided preliminary evidence that individuals with low perceived risk in relation to COVID-19 may be key targets for behavior change interventions, and, as such, identifying participants with low perceived risk to target through intervention may be crucial to reducing community transmission in future outbreak scenarios. Further research with pre-registered hypotheses is recommended to test the moderating effect of risk perception on avoiding touching the face with unwashed hands in the context of the present intervention. Further research is also recommended to test the efficacy of the present intervention during a normal flu season– a period when hand hygiene behavior is important for limiting pathogen transmission, but without pervasive media coverage and public health messages prompting behavioral engagement, as with the COVID-19 pandemic. Results of such research would be transferrable to a large-scale pandemic, particularly for initiating faster and earlier adoption of protective behaviors in the instance of an outbreak.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Stephanie R. Smith, Martin S. Hagger, Jacob J. Keech, Susette A. Moyers and Kyra Hamilton declare that they have no conflict of interest.
Authors’ Contribution Stephanie Smith, Kyra Hamilton, Martin Hagger, Jacob Keech and contributed to conceptualisation. Stephanie Smith, Susette Moyers, and Jacob Keech contributed to data curation and formal analysis. Stephanie Smith, Martin Hagger, Jacob Keech, Susette Moyers and Kyra Hamilton contributed to investigation. Stephanie Smith, Martin Hagger, Jacob Keech and Kyra Hamilton contributed to methodology. Stephanie Smith, Susette Moyers and Jacob Keech contributed to project administration. Kyra Hamilton and Martin Hagger contributed to resources and supervision. Martin Hagger and Jacob Keech contributed to validation. Stephanie Smith served as lead for visualization and writing - original draft. Martin Hagger, Kyra Hamilton, Jacob Keech, Susette Moyers and Stephanie Smith contributed to writing – review and editing.
Ethical Approval All procedures, including the informed consent process, were conducted in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Transparency statements (1) The studies were pre-registered at Open Science Framework: Study 1 https://doi.org/10.17605/OSF.IO/3RH9U; Study 2 https://doi.org/10.17605/OSF.IO/RPK3A. (2) The analysis plans for each study was registered prior to beginning data collection at Open Science Framework: Study 1 https://doi.org/10.17605/OSF.IO/3RH9U; Study 2 https://doi.org/10.17605/OSF.IO/RPK3A. (3) De-identified data from this study are available in a public archive: https://doi.org/10.17605/OSF.IO/UQC6B. (4) Analytic code used to conduct the analyses presented in this study are available in a public archive: https://doi.org/10.17605/OSF.IO/UQC6B. (5) All materials used to conduct the study are available in a public archive: https://doi.org/10.17605/OSF.IO/UQC6B



