-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan E Butner, Cynthia A Berg, A K Munion, Sara L Turner, Amy Hughes-Lansing, Joel B Winnick, Deborah J Wiebe, Coordination of Self- and Parental-Regulation Surrounding Type I Diabetes Management in Late Adolescence, Annals of Behavioral Medicine, Volume 52, Issue 1, January 2018, Pages 29–41, https://doi.org/10.1007/s12160-017-9922-0
Close - Share Icon Share
Abstract
Type 1 diabetes management involves self- and social-regulation, with past research examining components through individual differences unable to capture daily processes.
Dynamical systems modeling was used to examine the coordinative structure of self- and social-regulation (operationalized as parental-regulation) related to daily diabetes management during late adolescence.
Two hundred and thirty-six late adolescents with type 1 diabetes (M age = 17.77 years, SD = .39) completed a 14-day diary reporting aspects of self- (e.g., adherence behaviors, cognitive self-regulation failures, and positive and negative affect) and parental-regulation (disclosure to parents, knowledge parents have, and help parents provide).
Self-regulation functioned as one coordinative structure that was separate from parental-regulation, where mothers and fathers were coordinated separately from each other. Mothers’ perceived helpfulness served as a driver of returning adolescents back to homeostasis.
The results illustrate a dynamic process whereby numerous facets of self- and social-regulation are coordinated in order to return diabetes management to a stable state.
Type 1 diabetes management in adolescence is a complex regulatory task wherein both individual “self and interpersonal “social” regulatory processes are critical to achieving optimal diabetes management [1, 2]. Self-regulation (i.e., the modulation of emotions, behaviors, and cognitions toward a goal) [3] and social-regulation (i.e., social resources that serve to modulate emotions, behaviors, and cognitions within the dyad or group) [4] processes have been linked with diabetes management in adolescents. For example, completion of adherence behaviors (e.g., monitor blood glucose levels, maintain healthy diet and exercise, adjust insulin doses as a function of blood glucose, eating, and activity levels) increases when adolescents are successful at self-regulating [5–7], including regulating emotions such as negative affect about diabetes management [7–9] and cognitions such as remembering to test and preventing distractions to testing [5, 9]. Diabetes management is also more optimal when adolescents engage in parental-regulation processes such as disclosing to parents so that parents can be knowledgeable about their diabetes management and provide support when needed [10, 11]. This social-regulation is integral along with self-regulation in promoting successful diabetes management.
Typically, type 1 diabetes management has been studied via static snapshots where management behaviors are predicted by individual differences in self-regulation and/or social-regulation. Optimal diabetes management requires multiple times per day collecting information regarding blood glucose (BG) values, carbohydrates consumed, and completed or planned exercise to make insulin dosage decisions aimed at maintaining relatively normal BG levels [12]. Thus, as self- and social-regulation take place multiple times per day concurrently, the typical snapshot approach does not capture the transactional way in which self-regulatory and social-regulatory processes move together throughout time, nor how self-regulation may relate to social-regulation (i.e., both adolescents’ attempts to seek assistance from parents and parents’ efforts to provide the help that is needed to support management).
The present study uses dynamical systems modeling—a series of analytic techniques for studying change processes—to examine diabetes management as a system, capturing the multidirectional relations of self- and parental-regulation (i.e., social-regulation involving parents), as they are associated with daily diabetes management during late adolescence. Late adolescence is a crucial time in development when parents are less involved than at earlier time periods to support diabetes management and adherence is deteriorating [13]. A dynamical systems approach is ideal to capture real-time transactional processes between adolescents and parents [14], similar to those that are likely to occur when families manage type 1 diabetes. Such models can identify what variables are drivers of change in self- and parental-regulation processes across time, allowing us to understand the stability of regulation within the diabetes management system. A dynamical system analysis of diabetes management addresses recent calls within both the diabetes [2] and broader behavioral medicine literatures [15] to examine adherence and health behaviors from a systems perspective.
As an example of the daily self- and parental-regulation processes that comprise the diabetes management system— processes that we will model from a dynamical systems perspective—imagine Morgan who struggles to test her BG throughout the day. On a school day with an important examination period beginning, she frequently has to regulate her negative affect about performance on the exams and finds herself regularly “forgetting to test.” Her mother and father become involved when Morgan discloses to her parents that she has not tested all day at school. With this knowledge about Morgan’s diabetes management, the next day they may assist her more (e.g., texting reminders to test), which seems to provide the support she needs to get her BG testing back on track. Understanding how facets of self-regulation move together through time and are linked to aspects of social-regulation in relation to mothers and fathers is important in understanding diabetes self-management.
Complexity and Coordination
Inherently, examining diabetes management as a complex system makes for a complex problem. Dynamical systems modeling approaches aim to capture the relationships among multiple variables simultaneously through time by characterizing a variable as a function of its changes on previous and future values [16]. Linkages between variables can then be examined for their predictive contribution to the future values of or changes in the other variables [17], generating a notion of how variables function together, as a system. For example, in the same way that autoregressive relationships are indicative of consistency across time, the extent to which parental-regulatory aspects of diabetes management predict changes in parental-regulatory aspects (predicting its own change) indicates the stability of parental-regulation over time. Further, the extent to which self-regulatory aspects of diabetes management predict changes in parental-regulatory aspects (known as coupling relationships) would be interpreted as an indication of a driving influence in the push-pull self-parental relationship.
The models proposed herein are based on theories of coordination [18]—how variables in the same system move together. Coordination builds upon the notion of values predicting changes into the future by considering what it means when two or more variables change simultaneously— the correspondence of changes rather than the correspondence of value. Under coordination, a specific variable is believed to contain both its own stable pattern through time (e.g., the longitudinal declines in adherence behaviors seen across adolescence) and the push and pull that comes from being coordinated with other variables in the system (e.g., day-to-day fluctuations in adherence linked to forgetting to test BG or feeling distressed).
Butner et al. [19] modeled such coordination of changes through a latent variable of the changes in multiple variables in the diabetes management system, including self-efficacy, self-control, and parental monitoring. Butner et al. [19] revealed in adolescents managing type 1 diabetes that changes in self-efficacy showed corresponding changes in behavioral self-control such that when one showed a positive change, so did the other. The inclusion of coordination using latent variables of changes allowed for the examination of different underlying coordinative structures among these processes. For example, while parental monitoring was coordinated between parents, it was unlinked from coordinated changes in self-efficacy and self-control.
Models of coordination can also identify drivers of coordination. That is, some variables may asymmetrically influence the coordinated process and, in turn, the stability of the system. These drivers have greater potential to push and pull the other components back to the overarching stable pattern. Further, such links can occur across coordinative factors potentially linking self- and social-regulation factors, even if these variables coordinate separately. For example, Butner et al. [19] found behavioral self-control could predict the coordination of the self while self-efficacy could not, suggesting that behavioral self-control may have been a key driver toward the stable changes in their coordinated patterns through time. Note that this is similar to a causal argument, but not actually one, in that systems models inherently assume bidirectional causal relationships, wherein the complex interactions among variables can result in the emergence of some variables functioning as key stabilizing factors [20].
Diabetes Management as Coordination
In the present study, we examined the dynamic processes of daily diabetes management through a daily diary and considered multiple facets of diabetes management focused on self-regulation (positive and negative affect, self-regulation failures, BG tests, problems with diabetes, adherence, and self-efficacy) and parental-regulation (disclosing to parents, parents’ daily knowledge of diabetes management, and parental support). Developmental theories suggest three different plausible models of how management components could move together with the family system across time.
Self- and Parental-Regulation are All Coordinated Together
Self- and parental-regulation could comprise one large coordination pattern, implying that both are governed by some general capacity of the adolescent (e.g., executive function) and/or the larger family system. That is, late adolescents who are better able to regulate themselves likely develop out of families that are also better able to provide support and monitor their adolescents [21]. Parent monitoring and knowledge are associated with better adherence and might play a role as a unified family system in fostering adolescent self-regulation related to completing diabetes management tasks [13, 22, 23].
Self- and Parental-Regulation Aspects Coordinate Together
Self-regulation could form one coordination pattern and parental-regulation another (the parents as a team), illustrating separateness between regulation occurring within the individual versus within their social system, consistent with Butner etal. [19] Parental-regulation involving adolescents disclosing to parents and parents having knowledge to assist when needed may be related [10] and form its own coordinative system. Separation between self- and parental-regulation could derive from the declines that occur in parents’ involvement in and knowledge of their child’s diabetes activities across adolescence [13, 24].
Self-Regulatory Aspects and Each Parent Could Coordinate Separately
In addition to self-regulation, the coordination of mothers and fathers may be separate, given their different proximity to the daily behaviors that comprise management, with mothers being more involved in daily management [25] For example, mothers are often more involved in the day-to-day management of children’s diabetes, while fathers are often involved when greater problems with diabetes management arise [26].
In addition to these coordination structures, we also explored whether some variables serve as drivers of the coordinated structure, allowing all aspects of the coordinated system to be drivers. Differences between mothers’ and fathers’ involvement led us to expect mothers would have more potential as a driving link between adolescent and social aspects of management.
To test these hypotheses, we examined the three alternative models of coordination using data from a larger longitudinal study, where late adolescents completed a 2-week end-of-day diary assessing multiple facets of self- and parental-regulation. Our approach was to utilize multiple indicators of behavioral (adherence, blood glucose checks, daily problems with diabetes), cognitive (self-regulation failures, self-efficacy), emotional (positive and negative affect), and social aspects of diabetes management (disclosure to parents, knowledge parents have, and help received from parents) to determine the underlying structure of how these variables change from 1 day to the next. We assessed the extent to which these 13 aspects of daily management moved together, testing multiple different underlying coordinative structures. We hypothesized that self- and parental-regulation would coordinate separately and that mother and father aspects of parental-regulation would coordinate separately given mothers’ greater involvement in daily diabetes management [25]. Although we had no particular hypotheses about what would drive self- and parental-coordination, we anticipated there would be identifiable links between parental- and self-regulation, especially involving mothers.
Methods
Participants
High school seniors with type 1 diabetes were recruited for a longitudinal study on diabetes and self-regulation during late adolescence and emerging adulthood. Participants were recruited from three outpatient pediatric endocrinology clinics in two southwestern US cities. Of the qualifying 507 individuals approached, 247 adolescents completed baseline assessments (see [10] for more details).
Adolescents were eligible to participate if they had been diagnosed with type 1 diabetes for at least 1 year (M length of diagnosis = 7.35 years, SD = 3.88), had English as their primary language, were in their final year of high school, lived with a parent (68.4% lived at home with both biological parents, 27.1% with one biological parent, and 4.5% lived with adoptive parents or grandparents), would be able to have regular contact with parents over the subsequent 2 years (consistent with objectives of the broader longitudinal study), and had no condition that would prohibit study completion (e.g., severe intellectual disability and blindness).
Consistent with the patient population at participating clinics, 75.2% of the full sample (N = 247) identified as non-Hispanic White, 14.2% Hispanic, 4.8% African American, and the remainder as Asian/Pacific Islander, American Indian, or more than one race. Patients were 17.76 years old on average (SD = 0.39) and 60% were female. Parents had a range of educational backgrounds, with 12.9% of mothers and 18.2% of fathers having a high school education or less, 37.2% of mothers and 25.1% of fathers with some college or a vocational degree, and 34% of mothers and 46.3% of fathers with a bachelor’s degree or higher.
The present study analyzed baseline data from participants who responded to the daily diary (N = 236). Adolescents in this subsample were 17.77 years of age (SD = 0.39) on average and had been diagnosed with type 1 diabetes for an average of 7.34 (SD = 3.88) years. In this subsample, 62% of adolescents were female, and 43% of patients reported using an insulin pump. Sixty-three percent of our analyzed sample was above the ADA age-specific recommendations (HbA1c < 7.5%) for glycemic control (M HbA1c = 8.27, SD= 1.62).
Procedure
The study was approved by the appropriate Institutional Review Boards, with parents providing informed consent and adolescents providing consent or assent. At an initial meeting, participants were consented and completed other measures for the broader study, and received instructions for completing a subsequent confidential online survey and daily diary procedure. The 14-day daily diary data were used for the present analyses. For measures of mother and father involvement, adolescents selected one mother and father figure to report on consistently across time. If adolescents had more than one mother or father figure, they selected the mother or father figure who was most involved in their diabetes care (97.2% of adolescents nominated biological mother and 90.9% nominated biological father). Each day, participants received a link to a confidential brief electronic survey with instructions to complete individually to indicate experiences in the past 24 h. To facilitate diary completion, adolescents received phone calls or text messages daily if they had not completed the diary by 9p.m. Adolescents were paid $50 for lab procedures and the online survey, and $5 for each daily diary completed.
Daily Diary Measures
All daily diary measures were created for the present study by the authors. To reduce burden and increase compliance, many scales utilized as few items as possible while maintaining adequate psychometric properties.
Self-Regulation
Daily Self-Regulation Failures
Adolescents reported daily on their experience of eight failures in diabetes self-regulation surrounding testing BG levels, which is a crucial and difficult daily adherence behavior (e.g., “Each time I was about to test my BG, I got distracted by something else.”) [5, 12] using a 1 (strongly disagree) to 5 (strongly agree) scale. A summed daily score was used, with higher values indicating more failures (M = 16.35, average number of days completed = 10.9). Inter-item reliability of the eight items was calculated via random intercept models, with both time and item treated as nested levels and was excellent (α = .98).
Daily Adherence
Teens rated their adherence to the diabetes regimen using six items from the Self Care Inventory [27] that reflect management behaviors that should be completed daily. Items were rated for how well teens followed recommendations for each behavior in the past 24 h using a 1 (did not do it) to 5 (did it exactly as recommended) scale (α = .97, M= 4.17, average number of days completed = 10.2).
Daily Frequency of BG Tests
Participants reported the number of times they checked their BG levels with their glucometer in the past 24 h (M = 3.74, average number of days completed = 10.5).
Daily Diabetes Problems
Participants completed a checklist of five diabetes-specific stressful events (i.e., problem with high/low blood sugar, forgetting or skipping a blood glucose test, taking wrong amount of insulin, feel bad because of diabetes, and problem with pump or continuous blood glucose monitor) derived from previous coding of open-ended descriptions of mother- and adolescent-reported diabetes events [28]. The number of diabetes problems was measured by counting the number of diabetes problems endorsed each day (M =1.16, average number of days completed = 12.2).
Daily Positive and Negative Affect
Participants rated how much they felt during the past 24 h nine items tapping negative affect (3 each reflecting depressed mood, anxious mood, and anger) and nine items reflecting positive affect (3 each reflecting happiness, interest, and contentment) developed by Cranford et al. [29] for use with daily diaries. Items were rated on a 1 (not at all) to 5 (extremely) scale, and average positive (α = .86, M= 2.86, average number of days completed = 11.0) and negative affect scores (α = .87, M = 1.79, average number of days completed = 11.0) were analyzed.
Daily Self-Confidence
Participants rated their confidence in their ability to manage diabetes each day using a 1 (not at all confident) to 5 (extremely confident) scale [25] (M = 3.70, average number of days completed =11.0).
Parental-Regulation
Adolescents completed parental-regulation items separately for mother and fathers to indicate disclosures to and help from parents each day. To measure daily adolescent disclosure about diabetes, participants responded yes or no to “Did you tell your mother/father about things that happened with your diabetes today, without her/him asking you?” (MMother = 0.27, Mfather = 0.17, average number of days completed for mother = 9.3, average number of days completed for father = 7.3). To measure parental knowledge, adolescents rated “How much does mother/father REALLY know about the diabetes problems you had today (e.g., high or low blood glucose)” on a 1 (nothing) to 5 (a lot) scale (MMother = 2.52, Mfather = 2.05, average number of days completed for mother = 10.7, average number of days completed for father = 9.7). To measure parental helpfulness, adolescents rated how helpful mother/father was in providing support for diabetes on a 1 (not at all helpful) to 5 (very helpful) scale (MMother = 2.71, Mfather = 2.27, average number of days completed for mother = 9.0, average number of days completed for father = 7.0).
Analysis Strategy
Our analytic strategy bridges two different approaches to estimating dynamical systems models—autoregressive and discrete change models. Vector autoregressive models are a way to represent coupling relationships between many simultaneous variables [30]. A future value of each variable is predicted by all the variables at a previous value in time. This establishes two types of relationships: the stability of the system through time (i.e., when a variable predicts itself) and a coupling relationship (when a variable uniquely predicts one of the other future variables).
We constructed discrete differences for each variable comprised of the variable at day t + 1 minus the variable at day t, for all days and all individuals. To capture coordination, we then constructed latent variables of these changes or latent coordination factors, which are manifestations of the changes in variables through time—how variables change together. For example, if aspects of the adolescent’s self- and parental-regulation all moved together, changes in the items would load onto the same latent variable. Coupling relationships were then captured through predicting the latent coordination factors as a function of the current variables, and stability information was captured in how a variable predicted its own change, after accounting for the coordination factor.
Multiple possible coordinated arrangements were tested as described above. The different loadings on the latent variables capture scaling differences in the changes. For example, if the loadings between two variables on the same latent coordination factor are 1 to 2, for every one unit change in the first variable, we observe a corresponding change of two units in the second. This relationship can be positive, implying increasing and decreasing together, or negative, implying when one increases, the other decreases.
We tested a total of three potential coordination factors. The first treated all 13 changes at a given time point as the manifestation of a single latent construct at that time point. The second separated the six parent items from the seven self items. The third divided the parent items into separate mother (three items) and father (three items) coordination factors. For all models, coordination factors were allowed to freely correlate. These covariances represent regular movement of the coordination factors with one another—though not consistent enough to collapse into a single representation. The tested lambda arrangements are in Fig. 1.
Three different factor models to capture latent changes. The manifest variables are discrete differences, and the one, two, and three-factor models further differentiate the roles of parents
How each variable predicts its own changes after accounting for the latent coordinations captures the inherent stability/instability of each variable through time. The scale of the coefficient changes such that a negative value becomes indicative of the variable showing an attractive pattern over time— homeostatic properties (higher values of a variable are associated with greater negative change). A positive coefficient becomes indicative of a variable showing a repulsive pattern over time—circumstances where the system is ever avoiding a value.
The combination of the presence of a latent coordinative structure and the potential for a variable to predict what remains after the coordination factor depicts the taxonomic representation of coordination observed. For instance, changes in adherence can be parsed into changes that are coordinated (the loading on the latent construct) and the portion that is not coordinated (what remains). If adherence were fully captured by the coordination latent variable, then there is nothing left to be predicted after accounting for the coordinated portion. If adherence is able to predict what remains after removing the coordinated portion, it suggests that some changes in adherence are consistent enough to be predicted by its previous values and some of the changes moved with the other coordinated variables. Finally, if changes in adherence did not load onto the coordination latent variable, then it is uncoordinated with the others.
In our model, driving relationships were then identified by variables uniquely predicting the latent coordination factors. This is the extent to which a preceding value is able to uniquely predict how all the variables change together in the future. Thus, they are also above and beyond the overall coordination relationships, since coordination factors are allowed to freely correlate.
This combined model resulted in a hybrid multilevel structural equation model, conducted in Mplus 7.23 [31]. All portions of the model were included simultaneously. That is, we had 13 changes (difference of next day value minus current day value) from each individual at each point in time, and the 13 values of the same variables (current day value) also for individuals at each point in time. The 13 changes formed latent coordination factors, the 13 same time variables predicted the portion of the changes not captured by the latent variables, and the 13 same time variables were also allowed to predict all the latent changes. All of this occurred within and across families in a multilevel model structure. Details of the model expressed in matrix algebra and further estimation choices are provided in Appendix 1.
On average, participants completed 11.2 diaries over the 14 days with missingness ranging from 1.2% (adherence) to a maximum of 36.8% (fathers’ helping). To account for these missing data, we utilized multiple imputations within Mplus under the assumption that the model accounted for the missingness (missing at random) [32]. In total, we generated 10 data files to counterbalance estimation efficiency with model runtime.
Very little has been published to the best of our knowledge on indications of model fit for hybrid multilevel SEM models, and there is a reason to question the interpretation for many fit indices under this complicated circumstance. We therefore relied on the Bayesian Information Criterion (BIC), which can be used for comparing both nested and non-nested models where a lower value indicates model preference. Since our MI procedure provided 10 BIC values for each model, we utilized a criterion of BIC differentiation rather than absolute BIC value. That is, we examined the extent to which the values overall were better or if they were much more difficult to differentiate. This logic is much closer to the Bayes Factor of which the BIC is a rough estimate [33]. This, in combination with a preference for parsimony, allowed us to identify the preferred coordination factor structure.
Results
In all 10 datasets, the BIC values for three different coordination factors resulted in lower values (by a difference in BIC values of at least 1000). We therefore report the three-factor solution. The matrix of loadings (L from Appendix 1) and covariances among coordination factors is provided in Fig. 2 showing parameters in all the expected directions. The signs of the loadings for each coordination factor suggest that coordination in each case is scaled to higher values, indicating changing toward better management. The positive relationships among the coordination factors suggests that, though the self, mother, and father showed some correlation through time, these relationships still grouped into three distinct coordinated components. Overall, this is consistent with self-regulation having a distinct role from parental-regulation involving mother and father in the diabetes management system.
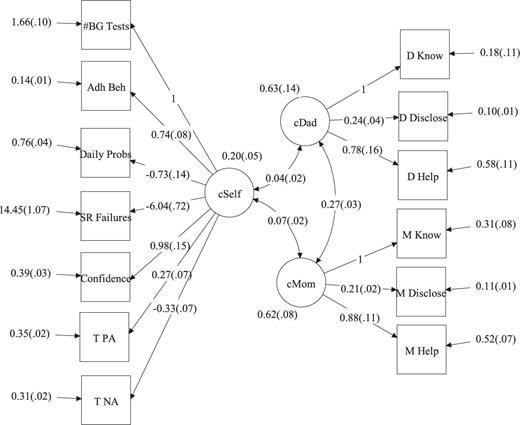
Loadings from final model. All variables are discrete differences of future minus current. Standard errors shown in parentheses
Figure 3 includes a figure of the own and coupling effects that surpassed significance criteria of alpha = .05, two tailed while Appendix 2 provides a table of all the individual coefficients. Every variable showed a substantial “own” effect, which was negative. This has two implications. First, changes in all variables loaded onto a coordination factor, and all variables maintained the ability to predict what remains in the changes after accounting for this coordination. This means the coordinative relationships did not dominate the patterns in each variable through time; instead, we are observing patterns that are a combination of their own tendencies and the coupling relationships slipping into and out of changing together. Second, since all the own effects are negative, it suggests that we are observing a stable system—each variable has attractive properties.
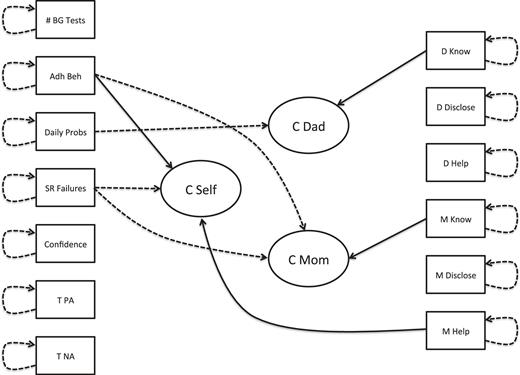
Network representation of relationships. Only those significant at alpha = .05, two tailed are shown. Variables at the beginning of arrows are current values, while the same variable at the head of an arrow is the discrete difference (future minus current). Solid lines represent positive relationships, and dashed lines represent negative relationships
For the self-coordination factor, both higher levels in adherence and lower levels in self-regulation failures predicted increases in the coordinated portion of the self-regulatory items. That is, above and beyond the other relationships, these variables continued to predict future shared changes. Coupling relationships like this are sometimes interpreted as representing driving relationships, in that they are particularly important in guiding coordinated changes across all variables in the system. Mothers’ help also predicted the coordinated changes in the self-component. This is consistent with mothers playing a particularly important role in contributing to coordination among the self-regulation variables, and, notably, this is above and beyond the other variables and the covariation of the coordination factors. No individual father’s item uniquely predicted the self-coordination factor. However, this does not mean that fathers had no contribution. Rather, such contributions were not unique or were captured through shared movement among the coordination factors (observed in the covariances).
For the parental-regulation coordination factors, parental knowledge predicted both mother and father coordination above and beyond the other relationships. This suggests that parents’ knowledge of their adolescent’s diabetes management activities is a key driver for both mother and father movement up and down, helping stabilize and destabilize the system. However, the arrangement of self-regulation items predicting each parent’s coordination factor was quite different. For mothers, higher values in both adherence and self-regulation failures predicted lower values of the mother’s coordination factor. This is unexpected in that these two measures are reverse-scaled (higher adherence is better management and lower self-regulation failures is better management). However, fathers’ coordination factor was only predicted by the total number of diabetes problems the late adolescent experienced that day (fewer problems predicted higher values in the fathers’ coordination factor).
Discussion
This dynamical systems perspective to diabetes self-management yielded several novel insights. First, during late adolescence, aspects of behavioral, cognitive, and emotional components to diabetes self-management functioned as one coordinated structure, supporting broad notions of self-regulation [3]. Second, these aspects of self-regulation coordinated separately from aspects of parental-regulation involving mothers and fathers in the late adolescent’s diabetes management activities, consistent with the developmental trend toward more independent self-management across adolescence [13, 24]. Despite the fact that self- and parental-regulation involving mothers and fathers were distinct, they were positively correlated, suggesting that they were all changing together. Third, all aspects of self- and parental-regulation had substantial effects of predicting their own changes above and beyond coordination, suggesting that each aspect was both distinct and connected with the others. Finally, there were important connections between parental-regulation (i.e., mothers’ perceived helpfulness) and self-regulation, indicating that mothers’ help drives the coordination of adolescents’ self-regulation.
The results support the view that processes related to self-regulation are coordinated as a system. From this perspective, the behavioral, cognitive, and emotional aspects of diabetes self-management all influence one another and help maintain the status quo. This is further supported by all the self-regulatory measures having a negative prediction of what remained after accounting for coordination, consistent with attractor patterns [19]. Such stability through time implies that if one were to change one variable such as adherence behaviors, other coordinated variables (e.g., cognitive and emotional aspects), and the higher order coordination pattern would move to re-stabilize adherence behaviors toward its more common homeostatic pattern. Thus, it is important to identify variables that drive the coordination of the system.
Within the self-regulation coordination factor, two such internal drivers were identified. Greater daily self-regulation failures were associated with changes toward lower levels of self-regulation, whereas greater daily adherence behaviors were associated with changes toward higher self-regulation. The daily self-regulation failures measure captured cognitive failures related to BG testing (forgetting to test, failure to initiate testing when motivation was low) and is related to broader self-reported problems in executive function and attention [5]. These cognitive failures may be especially problematic, as they may initiate changes in other aspects of self-regulation, such as undermining adherence behaviors and increasing negative affect and daily problems. Daily adherence behaviors themselves may be a key driver, as the successful engagement in such behaviors may support other aspects of regulation such as increasing self-efficacy, consistent with the Social Cognitive Theory [34].
Although there were both cognitive (i.e., SR failures) and behavioral (i.e., adherence) drivers, it is notable that there were no emotional drivers. These findings reveal that affect is an important component of diabetes self-regulation and are consistent with evidence that both positive and negative affect are associated with numerous aspects of daily diabetes self-regulation (e.g., self-efficacy, perceived competence in dealing with diabetes problems, and adherence behaviors) [7, 9, 35]. The absence of a driver effect indicates that affect did not display a unique contribution to self-regulation, or its contribution was captured through shared movement among other variables in the coordination. Affect and affect-regulation have been argued to occur in tandem with the self-regulation of behavior, with affect providing an important feedback function that aids in goal prioritization (e.g., positive affect indicates goal progress is acceptable so that limited resources can be shifted elsewhere) [36]. Future research that measures these nuanced aspects of daily goal striving as additional components of self-regulation may reveal a different role for affect in the daily dynamics of diabetes self-regulation.
Social regulation as captured through adolescents’ reports of mothers and fathers coordinated separately from self-regulation, with mothers and fathers being distinct from one another. These distinctions in parental roles for diabetes management are consistent with previous findings in younger adolescents where mothers and fathers had different perceptions of an adolescent’s competence and independence [37], but only mothers’ discrepancies from the adolescent related uniquely to metabolic control. Similarly, adolescent disclosures to mothers (but not to fathers) [10] and mothers’ (but not fathers’) efforts to persuade her adolescent to engage in better daily adherence were associated with better daily diabetes outcomes [25].
Within each parental coordination factor, adolescents’ report of the parent’s knowledge was a driver of the coordinated changes. This suggests the importance of parental knowledge in capturing changes in parental-regulation across days, potentially because parental knowledge captures an essential prerequisite for their help. Berg et al. [10] demonstrated that parental knowledge was obtained partially through adolescent diabetes disclosures, making it somewhat surprising that disclosure was not a driver in the parental-regulation coordination factors. Because our late adolescents were still living at home, parents may have gained knowledge through other means than adolescent disclosures (e.g., observing their adolescent’s diabetes activities). Nevertheless, the structural model of coordination clearly shows that disclosure and helpfulness are part of the coordination factor for both mothers and fathers, indicating the importance of all components for social regulation.
When examining the relationships between the self and parental aspects of diabetes management, mothers’ help—but not fathers’ help—provided additional prediction of the self-coordination factor, suggesting it is a driver to the adolescent’s self-regulation. This is consistent with our expectations of mothers functioning “in the trenches” with late adolescents, while fathers take an important, but more distal role. Further evidence of this interpretation comes from the differential aspects of the self that predicted the mother and father coordination factors. Both adherence behaviors and self-regulatory failures were drivers of the mother coordination factor, while only the number of daily diabetes problems was a driver of the father coordination factor. Fathers may thus be pulled in primarily when larger problems arise in the process of daily diabetes management [25, 38, 39].
Unexpectedly, self-regulation failures and adherence had different driver associations with the mother coordination factor, compared to their associations with the self-coordination factor. As expected, lower self-regulation failures were drivers of increases in both self-coordination and mother coordination. Thus, when adolescents reported fewer self-regulatory failures, they displayed subsequent increases in coordinated aspects of both self-regulation (e.g., increases in BG checks, self-efficacy, adherence, and positive affect) and parental-regulation (e.g., increases in disclosures to mother, mother’s knowledge and help). In contrast, higher adherence behaviors were drivers of increases in self-coordination but of decreases in parental-regulation. This unexpected pattern of results with respect to adherence could reflect a compensatory relationship. As adherence increases, mothers’ involvement could become less coordinated, as the processes of disclosure, knowledge, and helpfulness may need to be reorganized to reflect adolescents’ greater competence in self-management. Alternatively, this unexpected pattern could be one of over-controlling in that these models are capturing 13 simultaneous variables. The extent to which this replicates in future studies is of particular importance for helping elucidate this unexpected pattern.
One interesting future research direction will be to examine the extent to which the pattern of relationships across self- and parental-regulation hold as these late adolescents transition out of the household, when propinquity between parents and the young adult become less pronounced. By design, our sample of late adolescents was in their senior year of high school and still living with their parents. As late adolescents transition out of the parental home, social-regulatory opportunities to involve parents in their diabetes management are likely to be disrupted and may become completely separated from self-regulatory aspects. Given the difficulty of diabetes management, it is also plausible that the young adult may stay within the household longer to extend the possible social support parents are providing. Investigating such interplays during a transition period is paramount so as to understand how these transitions might function more smoothly to support diabetes management.
The results should be interpreted in the context of some limitations. First, self-report data from late adolescents (high school seniors) were used. Different results could occur with more objective measures or parent reports of diabetes self-regulation. It is also quite likely that the dynamics of diabetes self-management are fluid across age, so results may differ if younger or older participants are studied. Second, we examined these processes only at the end of the day, even though they likely vary throughout the day. Ecological Momentary Assessment (i.e., measures gathered throughout the day) will be important to understand fully the dynamic nature of these change processes across time. Finally, latent variables are always contingent upon what measures are included to reflect their manifestations. Our choice of using disclosure, helping, and knowledge to represent the social regulation of a parent, for example, may be one where the unique contributions of disclosure do not stand out while knowledge does. In this respect, as with all structural equation models, its description reflects the measures chosen.
In sum, this dynamical systems perspective to self-management of diabetes captures how daily processes are affected by aspects of self- as well as of social-regulation. By examining multiple variables through time, it is possible to observe the intertwined nature of their relationships. Further, the integration of self- and parental-regulation is paramount among late adolescents, providing evidence that managing a chronic illness is a family affair even as adolescents mature and become increasingly independent. Understanding how the different components of self- and parental-regulation isolate and consolidate developmentally recasts the operational nature of daily diabetes management closer to the theories of how individuals function within family systems [14]. The dynamical systems approach holds promise for moving the family system toward better diabetes management by shifting a system as opposed to failing, because the entire system resists the intervention.
Compliance with Ethical Standards
Author’s Statement of Conflict of Interest and Adherence to Ethical Standards Authors Butner, Berg, Munion, Turner, Hughes-Lansing, Winnick, and Wiebe declare that they have no conflict of interest with the project. All research was conducted under the guidance and oversight of the University of Utah, University of California at Merced, and University of Texas Southwestern Institutional Review Boards.
This work was supported by the National Institute of Diabetes and Digestive and Kidney Diseases at the National Institutes of Health (grant number R01 DK092939).
Appendix 1
where D is the vector of changes at each point in time for each family (the matrix is 13 × 1 at time t, family i), L is the lambda matrix (order is 13 × the number of latent coordination factors), or matrix of loadings of the form specified in Fig. 1. C is the matrix of coefficients of each variable predicting each latent coordination factor (number of latent coordination factors by 13). This matrix is fully estimated. V is the vector of values for each variable at each point in time for each family (13 × 1 for a given point in time and a given family). M is the vector of coefficients for each variable predicting its own changes post-multiplied by the identity matrix to turn it into a diagonal matrix and multiplied by the vector of values for each variable at each point in time. Z is the vector of estimated intercepts, and e is the level one residuals.
Implicit to this matrix equation is the inclusion of a covariance matrix of the latent coordinations at level 1 which was freely estimated. To provide metrics for each latent construct, we utilized a marker variable strategy, fixing one marker variable for each latent coordination factor. This established a metric for the coordination factors but also a metric for the loadings. Also implicit is the latent error variance/covariance matrix of the differences at level 1, which only allowed for each item to have its own residual variance—capturing the variances of the e vector. All random effects not specified were fixed to zero for ease of estimation of the 13 simultaneous variables.
Appendix 2
| Items predicting changes . | Teen . | Mother . | Father . | Own change . |
|---|---|---|---|---|
| Number of BG tests | 0.005 (0.009) | −0.003 (0.015) | 0.012 (0.018) | −0.383 (0.037)* |
| Self-regulation failures | −0.01 (0.003)* | −0.011 (0.005)* | −0.005 (0.005) | −0.348 (0.025)* |
| Average daily SCI | 0.096 (0.03)* | −0.084 (0.039)* | −0.112 (0.078) | −0.364 (0.025)* |
| Total non-pump diabetes stressors | 0.015 (0.017) | −0.046 (0.024) | −0.065 (0.031)* | −0.493 (0.03)* |
| Daily average PA | −0.002 (0.021) | 0.011 (0.037) | −0.016 (0.045) | −0.363 (0.027)* |
| Daily average NA | −0.051 (0.028) | 0.001 (0.038) | −0.014 (0.046) | −0.474 (0.028)* |
| Confidence in diabetes management | −0.008 (0.019) | 0.071 (0.037) | −0.046 (0.049) | −0.494 (0.027)* |
| Mother’sknowledge | −0.015 (0.022) | 0.149 (0.045) | 0.078 (0.053) | −0.537 (0.043)* |
| Mother’s help | 0.052 (0.023)* | 0.072 (0.04) | 0.043 (0.044) | −0.538 (0.039)* |
| Disclosure to mother | 0.004 (0.046) | −0.078 (0.076) | −0.057 (0.081) | −0.62 (0.028)* |
| Father’s knowledge | 0.04 (0.024) | 0.067 (0.043)* | 0.141 (0.06)* | −0.475 (0.063)* |
| Father’shelp | −0.045 (0.025) | 0.041 (0.039) | 0.02 (0.502) | −0.443 (0.043)* |
| Disclosure to father | 0.006 (0.051) | −0.052 (0.09) | −0.09 (0.098) | −0.609 (0.03)* |
| Items predicting changes . | Teen . | Mother . | Father . | Own change . |
|---|---|---|---|---|
| Number of BG tests | 0.005 (0.009) | −0.003 (0.015) | 0.012 (0.018) | −0.383 (0.037)* |
| Self-regulation failures | −0.01 (0.003)* | −0.011 (0.005)* | −0.005 (0.005) | −0.348 (0.025)* |
| Average daily SCI | 0.096 (0.03)* | −0.084 (0.039)* | −0.112 (0.078) | −0.364 (0.025)* |
| Total non-pump diabetes stressors | 0.015 (0.017) | −0.046 (0.024) | −0.065 (0.031)* | −0.493 (0.03)* |
| Daily average PA | −0.002 (0.021) | 0.011 (0.037) | −0.016 (0.045) | −0.363 (0.027)* |
| Daily average NA | −0.051 (0.028) | 0.001 (0.038) | −0.014 (0.046) | −0.474 (0.028)* |
| Confidence in diabetes management | −0.008 (0.019) | 0.071 (0.037) | −0.046 (0.049) | −0.494 (0.027)* |
| Mother’sknowledge | −0.015 (0.022) | 0.149 (0.045) | 0.078 (0.053) | −0.537 (0.043)* |
| Mother’s help | 0.052 (0.023)* | 0.072 (0.04) | 0.043 (0.044) | −0.538 (0.039)* |
| Disclosure to mother | 0.004 (0.046) | −0.078 (0.076) | −0.057 (0.081) | −0.62 (0.028)* |
| Father’s knowledge | 0.04 (0.024) | 0.067 (0.043)* | 0.141 (0.06)* | −0.475 (0.063)* |
| Father’shelp | −0.045 (0.025) | 0.041 (0.039) | 0.02 (0.502) | −0.443 (0.043)* |
| Disclosure to father | 0.006 (0.051) | −0.052 (0.09) | −0.09 (0.098) | −0.609 (0.03)* |
Significant at alpha = .05
| Items predicting changes . | Teen . | Mother . | Father . | Own change . |
|---|---|---|---|---|
| Number of BG tests | 0.005 (0.009) | −0.003 (0.015) | 0.012 (0.018) | −0.383 (0.037)* |
| Self-regulation failures | −0.01 (0.003)* | −0.011 (0.005)* | −0.005 (0.005) | −0.348 (0.025)* |
| Average daily SCI | 0.096 (0.03)* | −0.084 (0.039)* | −0.112 (0.078) | −0.364 (0.025)* |
| Total non-pump diabetes stressors | 0.015 (0.017) | −0.046 (0.024) | −0.065 (0.031)* | −0.493 (0.03)* |
| Daily average PA | −0.002 (0.021) | 0.011 (0.037) | −0.016 (0.045) | −0.363 (0.027)* |
| Daily average NA | −0.051 (0.028) | 0.001 (0.038) | −0.014 (0.046) | −0.474 (0.028)* |
| Confidence in diabetes management | −0.008 (0.019) | 0.071 (0.037) | −0.046 (0.049) | −0.494 (0.027)* |
| Mother’sknowledge | −0.015 (0.022) | 0.149 (0.045) | 0.078 (0.053) | −0.537 (0.043)* |
| Mother’s help | 0.052 (0.023)* | 0.072 (0.04) | 0.043 (0.044) | −0.538 (0.039)* |
| Disclosure to mother | 0.004 (0.046) | −0.078 (0.076) | −0.057 (0.081) | −0.62 (0.028)* |
| Father’s knowledge | 0.04 (0.024) | 0.067 (0.043)* | 0.141 (0.06)* | −0.475 (0.063)* |
| Father’shelp | −0.045 (0.025) | 0.041 (0.039) | 0.02 (0.502) | −0.443 (0.043)* |
| Disclosure to father | 0.006 (0.051) | −0.052 (0.09) | −0.09 (0.098) | −0.609 (0.03)* |
| Items predicting changes . | Teen . | Mother . | Father . | Own change . |
|---|---|---|---|---|
| Number of BG tests | 0.005 (0.009) | −0.003 (0.015) | 0.012 (0.018) | −0.383 (0.037)* |
| Self-regulation failures | −0.01 (0.003)* | −0.011 (0.005)* | −0.005 (0.005) | −0.348 (0.025)* |
| Average daily SCI | 0.096 (0.03)* | −0.084 (0.039)* | −0.112 (0.078) | −0.364 (0.025)* |
| Total non-pump diabetes stressors | 0.015 (0.017) | −0.046 (0.024) | −0.065 (0.031)* | −0.493 (0.03)* |
| Daily average PA | −0.002 (0.021) | 0.011 (0.037) | −0.016 (0.045) | −0.363 (0.027)* |
| Daily average NA | −0.051 (0.028) | 0.001 (0.038) | −0.014 (0.046) | −0.474 (0.028)* |
| Confidence in diabetes management | −0.008 (0.019) | 0.071 (0.037) | −0.046 (0.049) | −0.494 (0.027)* |
| Mother’sknowledge | −0.015 (0.022) | 0.149 (0.045) | 0.078 (0.053) | −0.537 (0.043)* |
| Mother’s help | 0.052 (0.023)* | 0.072 (0.04) | 0.043 (0.044) | −0.538 (0.039)* |
| Disclosure to mother | 0.004 (0.046) | −0.078 (0.076) | −0.057 (0.081) | −0.62 (0.028)* |
| Father’s knowledge | 0.04 (0.024) | 0.067 (0.043)* | 0.141 (0.06)* | −0.475 (0.063)* |
| Father’shelp | −0.045 (0.025) | 0.041 (0.039) | 0.02 (0.502) | −0.443 (0.043)* |
| Disclosure to father | 0.006 (0.051) | −0.052 (0.09) | −0.09 (0.098) | −0.609 (0.03)* |
Significant at alpha = .05
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.






